- We might be in the age of vitrectomy, but we believe that scleral buckling is the treatment of choice for certain retinal detachments
- But which patients are the best candidates for a primary scleral buckle and how should surgery be approached?
- We overview when primary buckling should be considered and provide guidance on which techniques will help success, as well as when to avoid a primary buckle
- Welcome to scleral buckling 101 for the senior ophthalmology resident and the junior retina fellow!
Rhegmatogenous retinal detachment (RRD) repair is one of the most common indications for retinal surgery. A multitude of anatomical presentations exist and therefore it is best treated with an individualized approach as opposed to a standardized procedure. Over the past 25 years, pars plana vitrectomy (PPV) has gained favor with vitreoretinal surgeons and is being used increasingly more than scleral buckling (SB) for RRD repair (1). Why has PPV gained favoritism? A variety of elements come into play, including the increased availability of small gauge instrumentation, improved viewing and lighting systems, industry support, as well as economic factors. However, we believe that SB should remain the treatment of choice for certain types of primary RRDs, and that it should remain in the vitreoretinal surgeon’s armamentarium for years to come. As such, it is imperative that current and future retinal fellows gain the skills necessary to perform the procedure.
SB was first described in 1949 by Ernst Custodis, and was further popularized by Charles Schepens and Harvey Lincoff in the 1950s. Over the past six decades, SB principles and techniques have remained relatively unchanged. The technique favorably alters the geometry and physiology of the eye to help close and maintain closure of retinal breaks. Inward indentation of the eye in conjunction with externally applied cryotherapy or laser photocoagulation creates a permanent adhesion between the neurosensory retina and the retinal pigment epithelium (RPE). Furthermore, SB-induced indentation helps overcome the forces tending to detach the retina, including cellular epiretinal proliferation and the magnitude and direction of vitreous traction on the neurosensory retina (2). SB surgery is advantageous because, as well as treating existing retinal breaks, it also supports the vitreous base, which prevents new retinal tears (3). Additional advantages of SB over PPV include a lower incidence of cataract (which may help preserve accommodation in younger patients), fewer complications (such as endophthalmitis or choroidal hemorrhage), and no need for post-operative positioning or travel restrictions (4). But in this age of vitrectomy, which patients are best candidates for a primary scleral buckle?
Who and why?
In our experience, SB surgery should be strongly considered in patients presenting with specific scenarios, which are outlined below with our reasoning:- Young, phakic patients with no posterior vitreous detachment. Why? Avoids cataract formation. Moreover, induction of a posterior vitreous detachment (PVD) during PPV can be technically challenging and create iatrogenic retinal breaks.
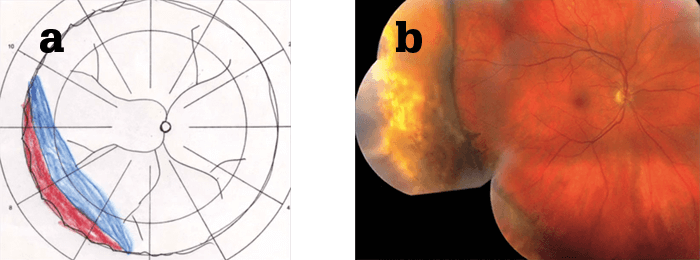
- Retinal dialysis. Why? Typically there is no associated PVD with dialysis. Further, given its anterior location, it can be difficult to visualize and therefore perform adequate vitrectomy in the area of dialysis.
- Very anterior break(s). Again, it is challenging to treat anterior retina with PPV.
- Patients with extensive lattice or multiple retinal breaks at the vitreous base. SB provides 360° support to the vitreous base and peripheral retina thereby preventing future tears.
- High myopia with contact lens intolerance in phakic, middle-aged patients with minimal or no cataract. SB will not cause significant cataract acceleration or anisometropia; however, PPV will accelerate the formation of cataract, which could complicate cataract surgical planning, as the most attractive refractive outcomes will induce significant anisometropia.
How? Buckling 101
Regardless of the treatment modality used to treat RRD, the single most important factor is to detect and treat all retinal breaks and areas of vitreoretinal pathology. Various techniques and materials can be used in SB surgery but the two primary principles remain consistent: i) Close retinal breaks by apposing the RPE to the sensory retina, and ii) Reduce dynamic vitreoretinal traction at sites of vitreoretinal adhesion.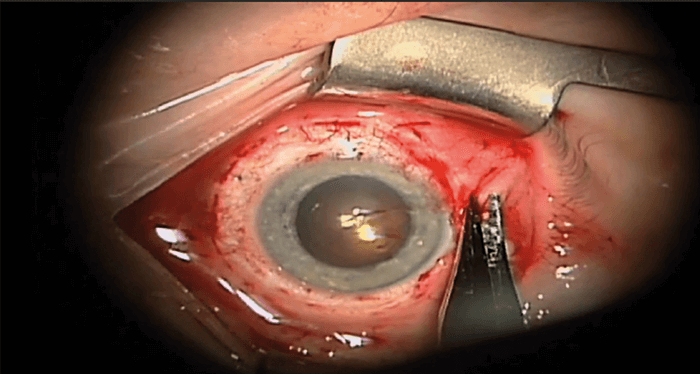
Worldwide, there is much variation in SB techniques and materials, but most procedures fall into one of three categories:
- Encircling circumferential buckle – 360° buckle. Used in cases with retinal breaks in three or more quadrants, diffuse retinal pathology (for example, lattice degeneration) or when there is concern about possible unidentified retinal breaks. These buckles are placed parallel to the limbus.
- Segmental circumferential buckle. Used in cases where the retinal breaks span less than 6 clock hours and all breaks are identifiable and treatable with cryotherapy or laser retinopexy. These buckles are placed in parallel to the limbus.
- Radial buckle. Used in cases with a single retinal break in an easily accessible location. Often for a large flap tear. These buckles are placed perpendicular to the limbus. A radial buckle may also be added to an encircling buckle in cases where the retinal tear is irregular or exhibits rolled edges.
When to avoid a primary buckle
Given the recent technological advances and excellent success rate of PPV, there are specific scenarios in which a SB is contraindicated:- Difficult visualization. Examination by indirect ophthalmoscopy is paramount during SB and thus any media opacities (for example, vitreous hemorrhage) limit the ability to treat with cryotherapy and/or laser.
- Posterior breaks. Difficult for external drainage of fluid and placement of a SB.
- Scleral thinning. Increased risk of globe rupture.
- Significant vitreoretinal traction. In cases with tractional membranes (e.g. proliferative vitreoretinopathy, proliferative diabetic retinopathy), PPV is the procedure of choice.
- Conjunctival peritomy and isolation of the rectus muscles.
- External localization of all retinal breaks. Use indirect ophthalmoscopy and a scleral localizer to mark each break on the external sclera.
- External drainage of subretinal fluid. Drainage of subretinal fluid should be performed in SB cases with a detachment that prevents adequate cryotherapy/photocoagulation treatment. This includes bullous RRD, chronic RRD, RRD with inferior retinal breaks, and in patients who are at risk of developing high intraocular pressure (for example, glaucoma or poor ocular perfusion).
- Treatment of retinal breaks with cryotherapy and/or photocoagulation.
- Placement of the SB.
- Re-examination of retina with indirect ophthalmoscopy. Ensure that all retinal breaks are treated with cryotherapy/photocoagulation and supported by scleral indentation. Also, confirm perfusion of the central retinal artery.
- Closure of Tenon’s capsule and conjunctiva.
In patients that are at high risk of developing proliferative vitreoretinopathy (PVR), it is appropriate to consider a combined PPV and SB procedure (5). A recent meta-analysis showed that the overall primary reattachment rate was significantly higher in PPV and SB than PPV alone, although the final reattachment rate was equally high in both groups (6). Therefore, we recommend consideration of a combined PPV and SB in patients who present with retinal detachment in two or more quadrants, retinal tears >1 clock hour, preoperative PVR, or vitreous hemorrhage. Alexander Ringeisen is a first-year retina fellow at VitreoRetinal Surgery, PA in Minneapolis, MN. Edwin Ryan is a vitreoretinal surgeon at VitreoRetinal Surgery, PA, and Associate Clinical Professor of Ophthalmology at the University of Minnesota. David Almeida is a vitreoretinal surgeon at Vitreoretinal Surgery, PA, Minneapolis, MN, USA. Almeida also writes a weekly blog, the Sunday Surgical Scrub, which can be found on his website davidalmeidamd.com.
