- As increasing numbers of LASIK patients become both presbyopic and in need of cataract surgery, there is a heightened demand and expectation for a good range of vision after cataract surgery
- Some compromises are inevitable when multifocal or accommodating IOLs are implanted in these patients
- The IC-8 small-aperture IOL is a new lens that uses the same small-aperture principle as the widely accepted KAMRA corneal inlay
- The lens is a good option for presbyopia patients, providing reliable visual quality across a range of distances.
Modern laser vision correction has captured the attention of the world. Millions of people have benefited from the procedure, but with these stories of success comes a heightened expectation of post-surgical outcomes. Maintaining a standard of excellent vision at all distances becomes complicated, though, once presbyopia becomes prevalent. And as ever-increasing numbers of patients who had undergone LASIK previously are now beginning to need cataract surgery, they’re not going to be happy settling for just good far vision while presbyopia robs them of their functional near vision.
We have Hermann von Helmholtz to thank for our present understanding of accommodation in the youthful, phakic eye (1). At rest, the supporting equatorial zonules maintain tension on the crystalline lens, flattening its central curvature to support distance focus. When the eye switches to near vision, the ciliary body constricts to release the zonular tension, allowing the anterior and posterior surfaces of the lens to bow outward and increase the converging power of the eye. This knowledge has paved the way for the development of a wide variety of intraocular lenses (IOLs) – multifocal and accommodating – that attempt to replace the eye’s natural loss of ability to adjust between near and far vision. Multifocal lenses either direct light in different ways to support vision at distinct distances, or have different zones within concentric rings for focusing at varying distances. Accommodating IOLs employ a hinged connection between the optic and supporting haptics that permits the lens to respond to ciliary body contraction, theoretically coming closer to natural accommodation. Choosing these options for patients with cataracts and presbyopia means facing a range of compromises, though, including incomplete range of vision, loss of visual quality due to induced glare and halo, and loss of binocular contrast.
Small aperture, but big advantages
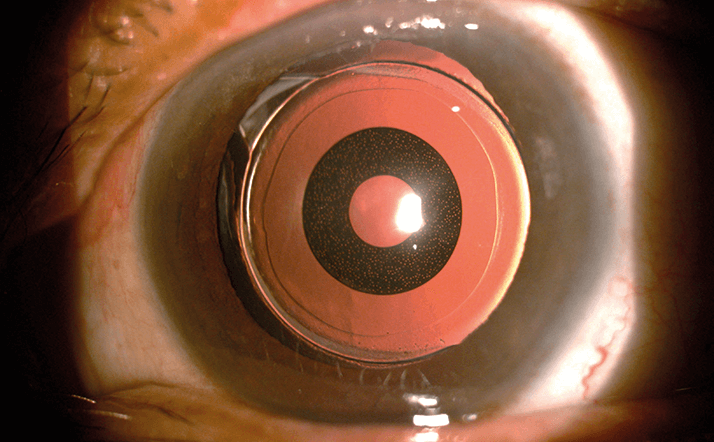
But there is hope – a recently completed proof-of-concept study indicates that another option may be on the horizon. The IC-8 small-aperture IOL, (AcuFocus Inc., Irvine, CA, USA, Figure 1), is a new lens that uses the same small-aperture principle as the KAMRA corneal inlay (also by AcuFocus), which, in my opinion, provides exceptional visual quality across a broad range of distances.The vision correction method employed by the KAMRA inlay has already gained widespread acceptance; when placed in the non-dominant eye, it has proven to be suitable for emmetropic and post-LASIK presbyopes, as well as monofocal pseudophakic patients. The aggregate results for this state-of-the-art procedure yield a mean uncorrected near visual acuity improvement of 4 lines from J8 to J2, and a mean uncorrected distance visual acuity change from 20/16 to 20/20 (2) – though of course, patient selection and surgical technique have been refined over time. The mean depth of focus in inlay eyes, assessed using a minus lens test, is 2.75 + 0.45 D at 60 cm and 1.98 + 0.21 D at 40 cm (3). Most importantly, patients treated with the KAMRA small-aperture inlay report being satisfied with their vision %95 percent of the time, while only 8 percent of these patients report using reading glasses for any amount of time (4). The IC-8 IOL, which is also intended for monocular implantation into the non-dominant eye, uses the same small-aperture principle as the inlay. It works by blocking unfocused peripheral light rays with an embedded opaque annular mask while allowing paraxial light rays through its central aperture. The lens is a single-piece hydrophobic acrylic lens, which contains a PVDF polymer mask of 3.23 mm in total diameter, with a 1.36 mm aperture. This opaque mask is 5 microns thick and contains 3,200 microperforations.
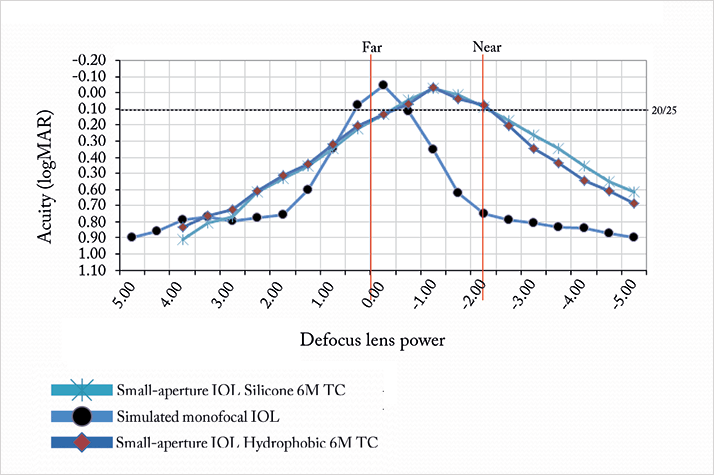
A small proof-of-concept study, using an earlier silicone IOL model, showed that monocular implantation of the small aperture IOL improved patients’ range of vision after cataract extraction (2). When the IOL is combined with -0.75 D of defocus, the result is an equivalent add power of approximately 2.25 D. The defocus curve for the IC-8 clearly shows the improved range of vision that can be achieved (Figure 2). As a result, patients experience a much more natural visual acuity, rather than the sudden increases and decreases that occur with a bifocal or multifocal lens.
I have implanted the IC-8 IOL into nine of my patients; after one year, they achieved a mean near visual acuity of J1 and a mean of 20/20 for both intermediate and distance visual acuity (5). Importantly, even in low light conditions, the IOL with the imbedded mask did not decrease binocular contrast sensitivity (6). Based on these promising early results, the manufacturer refined the IOL design and is now moving onto the next stage – initiating a post-market evaluation with the CE-marked IC-8 hydrophobic acrylic IOL. In my opinion, the small-aperture KAMRA corneal inlay has already shown to be an excellent option for presbyopia patients, providing reliable visual quality across a range of distances. Extending this principle to an IOL is an obvious next step and will bring the visual benefits of a small aperture to presbyopic patients with cataracts.
Günther Grabner is a Professor of Ophthalmology and Chairman of the University Eye Clinic, Paracelsus Medical University, Salzburg, Austria.
References
- H. Helmholtz, “Treatise on Physiological Optics”. Translated from the 3rd German ed. Southall JPC, ed. New York: Dover Publications (1962). Data on File. AcuFocus, Inc. F. Carones, “Assessment of the KAMRA Inlay Using Video Keratography and Corneal OCT: 2 Year Results”, presentation at the 2013 Congress of the ESCRS, Amsterdam, Netherlands, October 5–9, 2013. M. Tomita, T. Kanamori, G.O. Waring, et al., “Small-aperture corneal inlay implantation to treat presbyopia after laser in situ keratomileusis”, J. Cataract Refract. Surg., 39, 898-905, (2013). doi:10.1016/j.jcrs.2013.01.034. G. Grabner, “Four decades of cataract surgery: personal visions for the future”, Ridley Medical Lecture at the 2014 Congress of the ESCRS, London, UK, September 13–17, 2014. S. Manzanera, J. Marin, P. Artal, “Contrast sensitivity with a small aperture IOL evaluated with an adaptive optics instrument”, poster at the 2014 Congress of the ESCRS, London, UK, September 13-17, 2014.
