
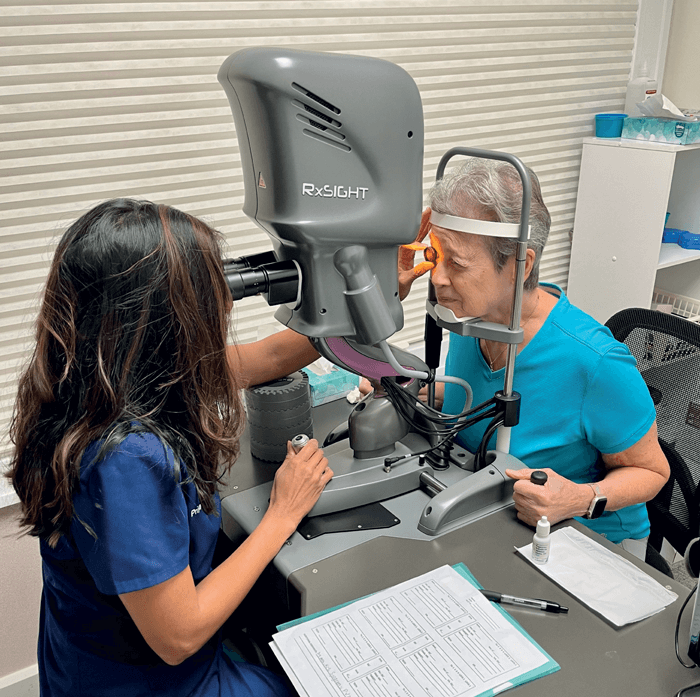
Although there have been many technological advances in cataract surgery since the first extraction was performed by French surgeon Jacques Daviel in 1747, it is still very difficult for surgeons to predict, pre-surgery, how their patients’ eyes will eventually heal. Revolutionizing the way cataract surgery is performed, the Light Adjustable Lens (LAL) from RxSight offers patients more control, customization, and confidence in their visual outcomes by allowing doctors to fine tune the lens prescription after surgery, rather than relying only on the choice of IOL power before surgery. The LAL was developed by Robert H. Grubbs, a Nobel Prize-winning scientist, using special photo-sensitive material that responds to UV light. Through a series of noninvasive UV light treatments using the proprietary RxSight Light Delivery Device (LDDTM), the technology enables patients to better customize their vision by changing the shape and prescription of the lens post-surgery. This novel approach – the first and only lens that can be customized after cataract surgery – means that patients are effectively able to “test drive” their visual outcomes to determine what tailored approach works best for them.
“The Light Adjustable Lens (LAL) has been a game-changer in my practice,” says Priya Mathews, a cataract, refractive,andcorneal surgeon based at the Center for Sight in Sarasota, Florida, who has a long-standing interest in addressing corneal blindness on a global scale. “I was initially motivated to use the LAL for two groups of patients in particular: patients with a previous history of refractive surgery and patients with mild-to-moderate corneal or retinal pathology,” she adds. “The LAL certainly met my expectations in terms of delivering the best possible outcomes with minimal refractive error in these patients, but I was also pleasantly surprised with how ideal it was for very detail-oriented patients and those who wanted to have some degree of control in their ultimate outcome after cataract surgery.”
Blended vision with the aspheric LAL, with refractive adjustments made in the post-surgery period - presents a major benefit to practitioners when compared to the traditional “monovision” route. “Blended vision allows the patient to read without moving their head or the reading material to find the exact focal point,” Mathews explains. “Personally, I do not offer a patient traditional monovision unless there’s a successful history of monovision in the past, especially if the near target is greater than -1.50 D. Sometimes patients who have done monovision for years can be unhappy after cataract surgery because they can lose some range in their near eye, due to the inability to accommodate after cataract surgery. Blended vision closes this “gap” and gives a wider range of focal points, particularly in the non-dominant eye. A vast majority of patients seem to easily adapt to some degree of difference between the two eyes...and if not, we can always tweak them back! That’s the beauty of this lens.”
While patients should be given the freedom to customize their vision, Mathews believes this freedom shouldn’t discourage surgeons from incorporating their own extensive experience into advising against any adjustments they feel are unwarranted. As for the specificities of targeting at surgery, she explains, “For my standard LAL patient, I aim for emmetropia in the dominant eye and -0.75 D in the nondominant eye before cataract surgery. If they have greater than 1 D of astigmatism, I perform femto LRIs (limbal relaxing incisions) at the time of cataract surgery to debulk the astigmatism and preserve more macromers for spherical adjustments.”

Meanwhile, Mathews’ strategy for the adjustment process after surgery is generally tailored toward the individual patient. “During the adjustment period, I dive into what the patient’s current experience is and what their goals are,” she says. “After surgery, patients typically end up about +0.50 D hyperopic of the goal, which is exactly what I want. For the first treatment, I target their initial goal. In addition, in the non-dominant eye, moving from the hyperopic to myopic direction with a goal of -0.50 or more myopia results in a further broadening of the LAL’s defocus curve. The secondary LDD treatment (if needed) is different for every patient, depending on what they want. Typically, two-thirds of my patients want more near, while one- third are happy where they are after the first treatment.” Then, Mathews adds, “Once the patient is happy and has thoroughly ‘tested’ their vision in multiple environments, including work, exercise, and home, we lock it in!”
Based on various patient testimonials (1, 2) and other real-world outcomes seen in clinical practice (3), the rate of patient satisfaction with the LAL process is impressive, and the second-generation LAL 2.0 has been reported as being “safe and efficacious even in challenging post- refractive clinical scenarios” (4). Priya Mathews herself confirms these reports: “Overall, I would say that I have a 99 percent satisfaction rate with the LAL. My patients have tailored their visual outcome according to what matters the most to them – therefore, what’s not to be happy about?”
References
- Slade & Baker Vision, “Locked into the Light Adjustable Lens: A Patient Experience,” (2023). Available at: bit.ly/43hlvQD.
- YouTube, “Light Adjustable Lens Patient Testimonial - Mary,” (2021). Available at: bit.ly/3PKNWDe.
- ECRS, “Light-Adjustable Lens Yields Positive Outcome,” (2021). Available at: bit.ly/44hVwty. 4. D V Folden, J R Wong, “Visual Outcomes of an Enhanced UV Protected Light Adjustable Lens
- Using a Novel Co-Managed, Open-Access Methodology,” Clin Ophthalmol, 16, 2413 (2022). PMID: 35957659.
