When it comes to glaucoma management, the last few years have seen an explosion in the number of treatment options available. As new devices emerge, it is important to understand how they differ from current offerings – and what they can bring to the table in terms of patient benefits. To find out more about the new PRESERFLO MicroShunt, we spoke with Julián García Feijóo, Chairman of the Department of Ophthalmology of the San Carlos Clinical Hospital, and Professor of Ophthalmology at Complutense University.
Please note: the content of this interview reflects the opinion of Prof. García Feijóo only; Santen has had no influence on the views expressed in this interview.
Could you tell me briefly about your practice?
I have both a private and a public practice. I work in one of the biggest hospitals in Spain, so we see a huge amount of activity – we do more than 1000 glaucoma surgeries every year.
Let’s talk about the PRESERFLO MicroShunt – how does it differ from other glaucoma devices?
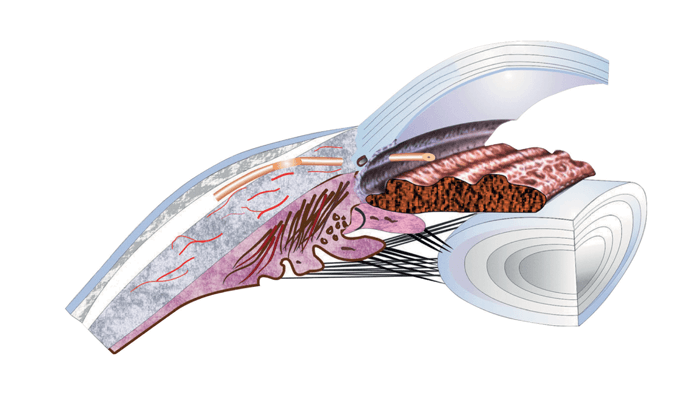
The PRESERFLO is a bleb forming device, so the idea is to connect the anterior chamber with the subconjunctival space – this is very similar to the XEN Gel Stent, for instance. The difference is that the PRESERFLO is implanted ab externo, rather than ab interno, so we can control the mitomycin C application area and its concentration. We can also manipulate and check the conjunctiva – that’s the beauty of the ab externo approach.
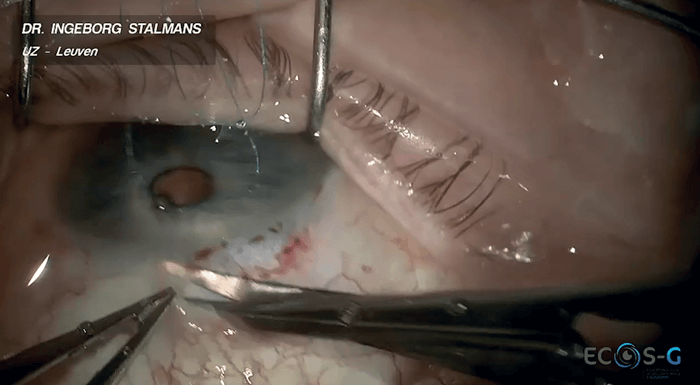
The PRESERFLO MicroShunt is made of material called SIBS, which makes it a highly biocompatible device. The armature is small, and the diameter and the length have been designed to avoid hypotony. Also the “fins” – an integral part of the design – minimizes the possibility of peri-tubular flow – this is very important because you have to completely introduce the fins in the pocket that you create during the procedure.
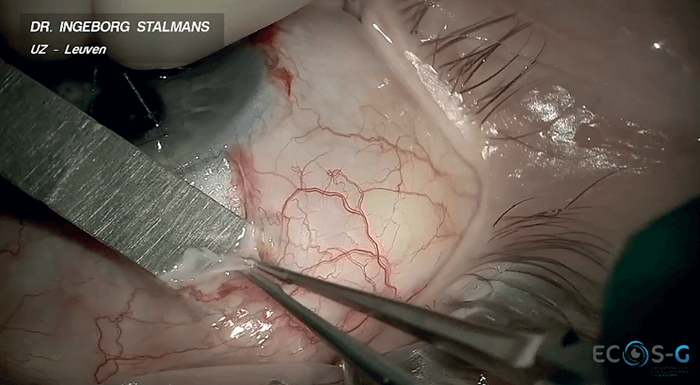
Could you go into more detail about the advantages of the ab externo approach?
The ab externo approach has numerous advantages especially in terms of the way mitomycin C can be used. When you apply ab externo, you open the conjunctiva and you can change the dose by changing the application time and the concentration of the mitomycin C. You can even use a larger or smaller area of mitomycin C, depending on the case.
You also took part in the INN005 Study Group trial. What were the headline results – and what are your opinions?
The study was a large-scale, two-year follow up study. Patients had primary open angle glaucoma that was uncontrolled on maximum medical treatment or with progression, so pressures had to be 18–35 mmHg. The end results were quite good, with an overall success rate of around 75 percent at one year, with a significant decrease in medication use. Mean IOP decreased from 21.7 mmHg to 14.5 mmHg at one year and 14.1 mmHg at two years. It’s good to know that after two years almost 74 percent of patients were off medications, and we didn’t really have serious adverse events. Furthermore, just 7 percent of patients needed additional surgery. Personally, another good thing about this study was that it confirmed my own feelings and personal experience – after all, I’d been using the PRESERFLO for some years before the study!
One interesting aspect of the study is that mitomycin C concentrations of either 0.2 or 0.4 mg/mL were used for 2–3 minutes. The study was not designed to compare mitomycin C concentrations, but we ended up with that data. In the 0.4 mg/mL cohort, 90 percent of patients were medication free after two years. So an additional lesson learned: when we increase the mitomycin C dose, the results are better.
How many MicroShunts have been implanted at your clinic – and what lessons have you learned?
We’ve implanted around 450 – possibly 500. First, we’ve learned to adjust the procedure a little over the years to improve the results in terms of IOP; for example, I already noted that I’ve increased the dose of mitomycin C to 0.4 mg/mL for 2–3 mins in almost every case. At this dosage, IOPs of around 10–12 mmHg are now possible with the microshunt.
In terms of safety, it’s important to completely insert the fins of the device in the scleral pocket. If you want to prevent hypotony – something that is always a concern in glaucoma surgery, you really have to use the device properly.
In short, my recommendations are to use the implant the way it should be used and use more mitomycin C!
Have you seen any long term complications in your patients as a result of endothelial cell count loss?
So far, there have been no big problems. And by “big problems” I mean corneal or endothelial transplantation. Surgical technique is very important in preventing endothelial loss. Especially when we insert the device in the anterior chamber. If it’s too close to the cornea, you have to do a new incision.
We have had to reposition a couple of implants that we thought were okay in the theater but weren’t positioned correctly. But, even in trabeculectomy, we use glaucoma medications and that has an impact on the endothelial cells. Obviously, the effect is greater with a glaucoma device – these are longer and the armature is larger, so it is something that we have to be careful about. In the study I mentioned earlier, there was no significant difference between trabeculectomy versus the MicroShunt in terms of the endothelium.
How do you manage your patients pre op?
I think we have to be very straight with patients. Sometimes it is not easy to decide what to recommend. For many patients, two or three options could be viable – in which case it may depend on the surgeon’s experience with one particular device. And sometimes it is the doctor’s intuition! Nevertheless, even if the clinic is busy, I try to spend time with the patient to explain why she or he needs surgery, as well as the options. For the PRESERFLO, if it’s a first surgery, I will explain the advantages and disadvantages of this option versus a trabeculectomy.
I’ve also seen some patients who come to the clinic asking for a particular device – “I want a MicroShunt” or “I want a XEN” – sometimes, that’s because they are afraid of trabeculectomy. In these cases, I take time and try to make them understand why a certain technique – or sometimes trabeculectomy – is a better option for them, particularly if they have narrow angle glaucoma.
I make my preference very clear – and explain my reasoning. But you have to take into account the patient’s specific situation as well; for example, if the patient doesn’t live in Madrid, post op care is not so easy, so I would recommend the PRESERFLO or another microshunt or even trabeculectomy.
Thinking specifically about the PRESERFLO MicroShunt, what key research would help you better understand the device and potentially improve outcomes even further?
One thing most surgeons want to understand is the reasons why any given device occasionally fails. In some cases, we may revise a bleb and find very thick tissue encapsulating the device. If we could profile the failure risk with genetic testing, cytokine levels or inflammation profiling, we would be able to adjust our techniques or choices.
Obviously research into better antifibrotic drugs would be welcome – but we’ve been trying to discover these drugs for more than 40 years – it’s like a quest for the Holy Grail!
Given my experiences, I would like to see more evidence exploring the comparative data between trabeculectomy and the PRESERFLO with a higher mitomycin C dose. As I said, I believe that with a higher mitomycin dose, the results are better.
Finally, even though we are focusing on microshunt as primary surgery here, I also have experience of implanting the MicroShunt in very different situations; for example, after failed trabeculectomy, after failed glaucoma device implantation or after surgery in congenital glaucoma patients. Therefore, I would like to see more data assessing the value of the MicroShunt in these clinical scenarios.

