- Transscleral cyclophotocoagulation (TSCP) destroys the ciliary processes, and lowers IOP by reducing aqueous humor production
- Although an effective procedure, TSCP is often considered a ‘last resort’ because of the discomfort of the procedure, the need for anesthesia or deep sedation, as well associated risks and complications
- As newer technologies become available, the role of TSCP should be reassessed such that it can be considered earlier in the treatment paradigm
- Using a segmented laser, TSCP can be used as an in-office procedure under local anesthesia.
Traditionally, cycloablation procedures to lower IOP have been reserved for patients at – or near – the limit of maximum tolerated medical or surgical therapy, or for patients with refractory glaucoma. One such procedure is transscleral cyclophotocoagulation (TSCP). Performed in the office or in the OR using an 810 nm laser and a transscleral laser delivery probe, TSCP involves ciliary body destruction by targeting the ciliary epithelium to reduce aqueous humor production and therefore lower IOP. Though effective, cyclophotocoagulation treatments can have some limitations and associated risks. One important limitation of traditional cyclophotocoagulation is the requirement for anesthesia. The treatment endpoint is ablation of the ciliary body in the superior and inferior regions, often marked by an audible ‘popping’ sound. As this is painful for the patient during treatment, anesthetic is required in the form of retrobulbar block, heavy sedation or general anesthesia in the OR. Although retrobulbar block is feasible, it comes with its own risks and potential complications, including retrobulbar hemorrhage, ocular perforation (especially in patients with high myopia or staphyloma), diplopia, retinal artery and vein occlusion, risk of perforating the nerve sheath or optic nerve damage. The TSCP procedure itself has also been associated with complications, such as hypotony, hyphema, vision loss, and inflammation that can lead to pain or discomfort after treatment.
As such, clinical decisions surrounding cyclophotocoagulation – and other cyclodestructive procedures – often balance safety and efficacy with quality of life, meaning that many physicians are not prepared to damage the ciliary body unless the prospect for disease progression and visual field loss are substantial. However, I believe that the role of TSCP for glaucoma management can be reassessed. With new techniques and technologies available it should no longer be considered only a ‘last resort’ treatment, but rather used earlier in the disease process and in patients who have good vision. MicroPulse technology – a treatment delivery mode in the Cyclo G6 laser console from Iridex – separates a continuous wave laser beam into segments, delivering targeted pulses of energy to the ciliary epithelium to modulate aqueous production. There is also some evidence that shows that segmented laser energy delivery augments the aqueous outflow pathway by constricting and expanding ciliary muscles (1). As the laser is applied with a duty cycle of 31.3 percent, energy is only delivered for around a third of the treatment application. Between pulses of energy, the tissue can cool, preventing a build-up of thermal energy and thermal spread. The reduction in overall energy also means that there is less pain and discomfort for the patient, which raises the potential to perform TSCP as an in-office procedure, using only local anesthesia – an approach we use for many of our patients.
In-office TSCP
In our clinic, we introduce MicroPulse TSCP to patients who are currently receiving IOP-lowering therapies. We find it a nice adjunct to most existing treatment approaches, and most of the cases I have performed are in individuals who have previously received laser trabeculoplasty. Previous argon laser trabeculoplasty (ALT) is not a contraindication, even though it yields destruction of the trabecular meshwork.Local anesthesia
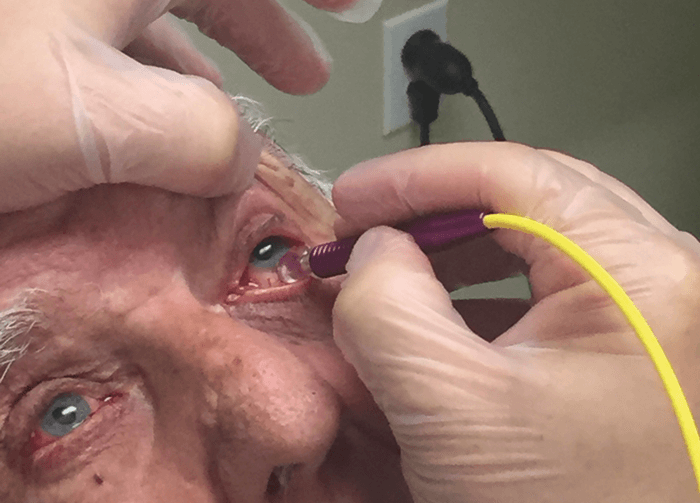
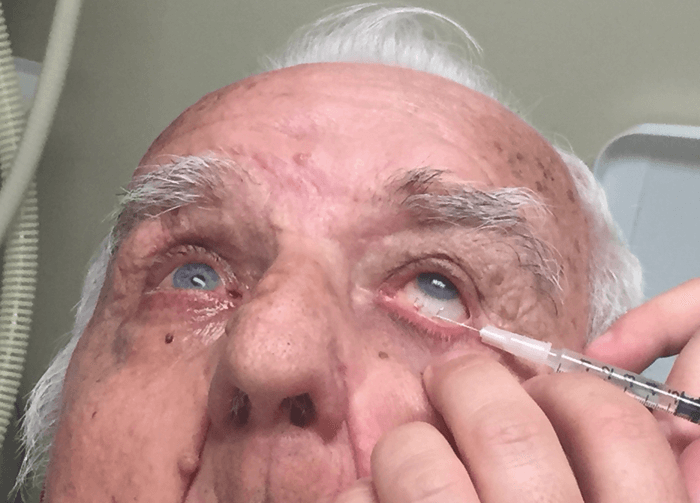
We begin the procedure by using a cotton tip to apply topical anesthesia to both the superior and inferior conjunctiva. We then inject local anesthetic (0.5 cc of 2 percent lidocaine with epinephrine) subconjunctivally to numb the globe, and allow it to diffuse for about 10 minutes. After the patient is comfortable, we set the laser at 2,000 mW of power with a 31.3 percent duty cycle.The treatment
Laser is applied in 10-second passes along the entire inferior or superior region of the eye, for a total of 90 seconds of treatment time per hemisphere. The 3 and 9 o’clock positions should be avoided because of the long ciliary nerves. Unlike previous versions of cyclophotocoagulation, there is no visible – or audible – tissue destruction to use as a treatment endpoint. Instead, treatment duration is decided at the surgical planning phase. For example, a treatment time of longer or shorter than 90 seconds may be used depending on the extent of IOP-lowering needed, and treatment duration can be titrated specifically to patients. Use of a lid speculum throughout the procedure is discretionary; some patients find it uncomfortable, and it is possible to simply hold the lids open while applying the laser.Post-procedure
After the procedure, we ask patients to apply a topical corticosteroid QID for one week. We typically see the patient back in the office at one week, one month, and three months post-procedure, depending on how their IOP is responding. As far as outcomes, we usually aim for patients to reach a target IOP rather than attempting a percent or numerical reduction in IOP; however, in our experience, 35 percent to 40 percent reduction in IOP can be expected.Our experience
We have found several advantages to performing in-office TSCP under local anesthesia. It is more time efficient than performing a retrobulbar block, or administering heavy sedation or general anesthesia – whilst also avoiding associated risks. There is no ‘downtime’ waiting for the OR staff to turn a room around or waiting for patients to be prepped for surgery. And that allows the treating physician to manage their time more appropriately. There is also less cost to the patient and insurance company because OR/ambulatory surgery center and anesthesia fees can be avoided. Moreover, as deep sedation or general anesthesia are not needed, we can verbally communicate with the patient during the procedure; not only do patients feel more comfortable as we apply the laser, but they can also inform treating staff if there is any pain or discomfort. So far, no patients have asked us to stop the procedure because of pain or discomfort. The procedure is non-invasive, and easily repeatable if necessary. In summary, as new technologies become available, it is time to consider the potential of TSCP as an in-office approach to treating glaucoma – and not just for patients who have a poor prognosis or refractory disease. David Gossage is a comprehensive ophthalmologist at Gossage Eye Institute and Optical, Hillsdale, MI, USA. Gossage reports that he receives compensation from Iridex for scientific lectures.References
- MA Johnstone et l., “Transcleral laser, ciliary muscle shortening & outflow pathway reorganization.” Invest Ophthal Vis Sci, 58, 3468 (2017).
