In my practice, most refractive surgery patients undergo either small incision lenticule extraction (SMILE) or transepithelial PRK (TPRK). A smaller percentage of high hyperopes and high myopes are offered hyperopic LASIK or phakic IOL surgery. Several years ago, I decided that offering simultaneous accelerated cross-linking (CXL) to my TPRK patients was an obvious choice to complement the biomechanical stability of TPRK.
A number of other authors have reported on combinations of CXL and excimer laser surgery in eyes with keratoconus, so it is very important to note that we only perform the TPRK-CXL procedure in eyes that are absolutely normal. We are not expanding the indications of refractive surgery to eyes with forme fruste keratoconus or suspect topography. Rather, we are adding the benefits of cross-linking and an extra measure of safety for those who already qualify for TPRK.
In this procedure, the TPRK ablation – combining PTK epithelial removal and PRK with the Amaris laser (Schwind) in a single step – is performed first (1), followed by accelerated CXL. The stroma is soaked with 0.1 percent riboflavin with hydroxypropyl methylcellulose solution (VibeX Rapid, Avedro) for 90 seconds and rinsed with chilled BSS. I then apply UV irradiation at a power of 30 mW/cm2 (total dose of 2.7 J/cm2) for 90 seconds, followed by mitomycin C 0.02 percent for 20 seconds.
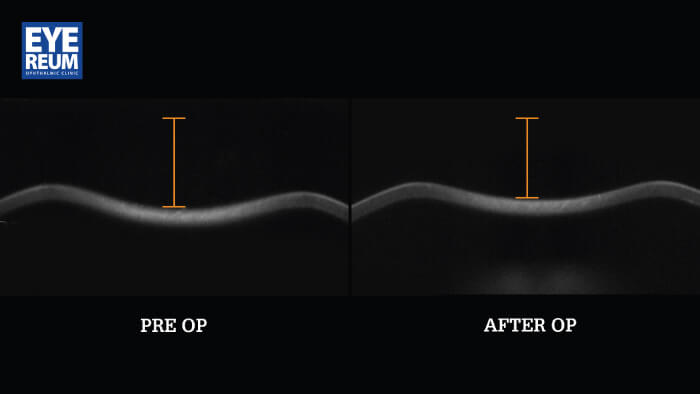
With this approach, I have found that we achieve greater biomechanical stability than standard TPRK without CXL (2, 3) and a biomechanically stronger cornea than after femtosecond laser LASIK with a 100-micron flap (4). My colleagues and I have evaluated corneal biomechanics across a number of studies using a dynamic Scheimpflug analyzer (Corvis ST, Oculus) that allows characterization of corneal biomechanical deformation in response to an applied air puff (Figure 1) (3, 4).
In addition, we have reported that there is less regression and epithelial hyperplasia with TPRK-CXL compared with standard TPRK (5). We also find earlier refractive stability and less residual spherical error in eyes treated with the combined procedure (2). No adjustments to the ablation profile are necessary to account for the effects of CXL. The predictability and refractive outcomes have been just as good or better with TPRK-CXL as with TPRK alone (2). I use the same postoperative protocols for TPRK with and without CXL.
Anecdotally, I find that the combined procedure heals slightly more slowly, but with less patient discomfort. We are in the process of studying pain and epithelial recovery time, and should have more information soon. Taking measures to prevent biomechanical weakening provides refractive surgery patients with an extra measure of safety, just as seat belts and airbags provide for us when driving a car. With TPRK-CXL, this can be accomplished with no detrimental effects on refractive outcomes.
References
- I Jun et al., “Comparison between wavefront-optimized and corneal wavefront-guided transepithelial photorefractive PRK in moderate to high astigmatism”, BMC Ophthalmol, 18, 154 (2018). PMID: 29940974.
- H Lee et al., “Comparison of outcomes between combined transepithelial photorefractive keratectomy with and without accelerated corneal collagen cross-linking: A 1-year study”, Cornea, 36, 1213 (2017). PMID: 28749894.
- H Lee et al., “Effect of accelerated corneal crosslinking combined with transepithelial photorefractive keratectomy on dynamic corneal response parameters and biomechanically corrected intraocular pressure measured with a dynamic Scheimpflug analyzer in healthy myopic patients”, J Cataract Refract Surg, 43, 937 (2017). PMID: 28823441.
- H Lee et al., “Changes in biomechanically corrected intraocular pressure and dynamic corneal response parameters before and after transepithelial photorefractive keratectomy and femtosecond laser-assisted laser in situ keratomileusis”, J Cataract Refract Surg, 43, 1495 (2017). PMID: 29335093.
- D Kang and S Kim, “Effect of corneal cross-linking on epithelial hyperplasia and myopia regression after transepithelial photorefractive keratectomy”, J Refract Surg, 35, 6, 354 (2019). PMID: 31185100.
