
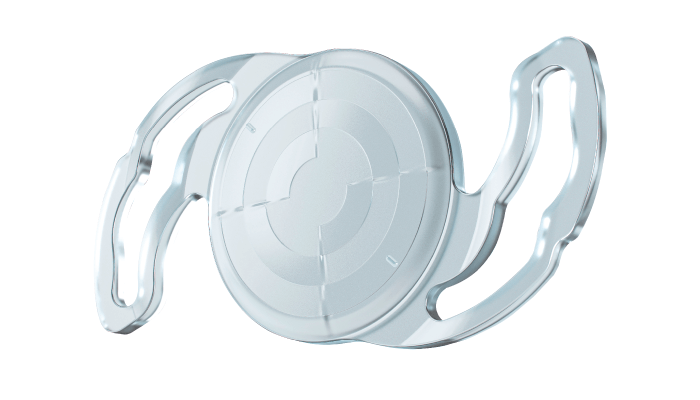
Youngsub Eom, Associate Professor, Korea University College of Medicine in Seoul, practices at the Department of Ophthalmology of the Korea University Ansan Hospital in South Korea, specializing in cataract surgery, management of ocular surface disease, dislocated IOLs, and corneal transplantation. Here, he shares his impressions of OPHTEC’s Precizon Presbyopic Toric IOL with CTF technology, which uses a multi-segmented optic with segments generating a wide range of foci, resulting in natural vision at all distances with significantly reduced photic phenomena, and TCT technology – the “Transitional Conic Toric Surface,” which blends into the aspheric surface of all meridians, leading to a broader toric surface.
Which IOL to choose?
In my clinic, halos and starburst photos are shown routinely to patients who want to undergo multifocal IOL implantation during cataract surgery (1). I explain that diffractive multifocal IOLs can provide better near vision, but could cause halos at night, and somewhat waxy vision. On the other hand, refractive IOLs provide clear distance vision, but could cause starbursts at night. If the patient wants clearer distance vision while potentially tolerating few starbursts, I select the Precizon Presbyopic IOL, and if the patient indicates they would tolerate waxy vision and the occurrence of halos at night, I recommend other multifocal IOLs. If the corneal astigmatism is 0.75 D or more in patients who have selected Precizon Presbyopic IOL, I choose Precizon Presbyopic Toric IOL.
Reducing halos and glare at all distances
Patients receiving diffractive MF IOLs often complain of waxy vision and discomfort due to halos and glare, but none of the patients who received the Precizon Presbyopic and/or Precizon Presbyopic Toric IOL in my hospital experienced waxy vision. And out of the 63 eyes in which I have implanted Precizon Presbyopic IOL, and of the 31 eyes in which I have used Precizon Presbyopic Toric, only three and two patients reported some halos or glare, respectively.
I feel that CTF technology provides natural vision at all distances, with sharp images from 5 m to near distance of more or less 33 cm, comparing favorably with competitor lenses, which produce blurry images at intermediate and near distances. In a previous study that evaluated the clinical outcome after implantation of Precizon Presbyopic IOL, visual acuity of 0.2 logMar or more was measured between defocus of +1.00 and -2.50 D as a result of binocular distance-corrected defocus curve (2). When residual cylinder and spherical equivalent are minimized, good vision at both near and distance can be achieved in patients with multifocal IOLs (3). For surgeons who are hesitant to use multifocal toric IOLs, the Precizon Presbyopic toric IOL, which has excellent tolerance for axis misalignment through TCT technology, can be used more safely to improve patient vision and satisfaction.
Patient outcomes: case study
My first patient who underwent Precizon Presbyopic Toric IOL implantation was the mother of a nurse working in my hospital. She had binocular NS3+ and CO3+ cataracts, and her right eye corneal astigmatism was -5.75D x 3°, while her left eye corneal astigmatism was -4.28 x 8° as measured by IOLMaster 500. Because of the large amount of corneal astigmatism, the Precizon Toric IOL was considered for its accurate astigmatism correction effect with TCT technology. The patient also wanted to improve her near vision. So the Precizon Presbyopic Toric IOL was chosen for her both eyes. The refractive error was -0.25 -0.50 x 170° for the right eye and plano for the left eye at postoperative six-month follow- up. Both I and the patient were very satisfied with the results of the surgery.
The patient had UDVA of 20/16 in the right eye and 20/12.5 in the left eye six months after surgery. Postoperative UNVA at 40 cm was J1 in both eyes, as was UIVA at 66 cm. The patient reported no photic phenomena (including glare, halos, hazy vision, blurred vision, distortion, or double vision) other than starbursts, which were occasional and caused no discomfort.
References
- Y Eom et al., Acta Ophthalmol, 95, e170 (2017). PMID: 27678470.
- Y Eom et al., J Refract Surg, 36, 740 (2020). PMID: 33170281.
- JW Kim et al., Graefes Arch Clin Exp Ophthalmol, 258, 1735 (2020). PMID: 32472200.
