Monofocal intraocular lenses (IOLs) have been positioned as the main refractive choice for cataract surgery, with the ever-increasing range of lens options offering surgeons unprecedented flexibility when choosing postoperative refractive outcomes. One of the primary benefits of alternative lenses is that they provide patients with quality, glasses-free vision in more than one focal plane. One way to achieve this is with multifocal lenses, but these come with a number of potential side effects, including reduced contrast sensitivity and an increased incidence of dysphotopsias (1). Another option is monovision with bilateral implantation of monofocal IOLs of asymmetric target refractions – but this is often associated with impaired binocular vision (2). Selecting the correct IOL for each unique eye has always been a challenge and the broad selection of IOLs surgeons now have at their fingertips enables more personalization than ever. Extended depth of focus (EDoF) IOLs, a relatively new contender in the space, may offer an opportunity for clear, functional vision at a range of working distances, ultimately providing a more satisfactory patient experience.
Recently, we conducted a prospective single-arm trial of patients undergoing bilateral implantation of a four-point haptic, hydrophilic acrylate, EDoF IOL with hydrophobic surface properties, a smooth microphase design, and a diffractive anterior surface design with an optical light bridge to provide satisfactory functional vision over a range of distances through the continuous extension of the range of focus; the aberration-neutral aspheric design and advanced chromatic aberration correction additionally optimize contrast sensitivity. We explored visual outcomes, contrast sensitivity, reading performance, and patient satisfaction and found that, after one year, most patients had an uncorrected distance visual acuity (UDVA) of 20/20 or better and uncorrected near visual acuities (UNVA) of N6 or better (3). The results demonstrate that the EDoF IOL provided good uncorrected near and far visual acuity outcomes. However, it is important to consider what factors influence EDoF lens outcomes and which patients are ideally suited for such IOLs.
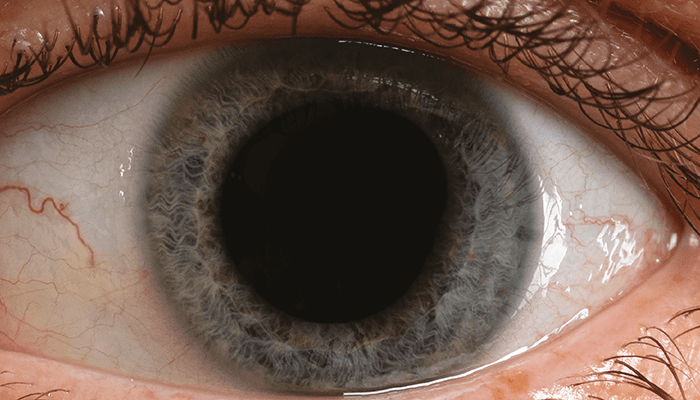
There is solid evidence to suggest that visual outcomes depend on several factors, such as coexistent pathology, axial length, anterior chamber depth, and zonular stability (4). However, preoperative mesopic pupil size is also important when considering EDoF lenses. To illustrate its potential effect on patient outcomes after EDoF IOL implantation, we have selected two case studies from the aforementioned study.
The first is a 60-year-old retired male who is overall healthy and leads an active lifestyle. His visual tasks include playing golf, following the stock market, working on computers for approximately four to five hours daily, and reading novels. Before surgery, this patient had grade II nuclear sclerotic cataracts (NS2) and posterior subcapsular cataracts (PSC) in his right eye and NS3 and PSC in his left eye, with insignificant posterior findings. His preoperative corrected distance visual acuity (CDVA) was 6/9 and 6/18 for the right and left eye, respectively; his corrected near visual acuity (CNVA), using +2.50 DS, was N6 for the right eye and N10 for the left. The preoperative mesopic sizes of the patient’s right and left pupils were relatively large at 5.16 mm and 5.59 mm; the left was the largest pupil in the cohort. Through biometry, we calculated that an IOL power of +19.50 D would achieve emmetropia in both eyes. Our findings one month after surgery included a UDVA of 6/5, UIVA of 6/6 at 60 cm, and UNVA of N8 in both eyes. Binocularly, he had a UDVA of 6/5 and UNVA of N6. The patient was highly satisfied with his distance vision and satisfied with near and intermediate vision, but found it inconvenient that he still needed glasses to read very small print.
The second case is that of a 62-year-old female, who is also generally healthy and active. Her visual tasks include driving during the day, hiking, and reading e-books on a tablet computer. The patient had NS2 and dense PSC with early AMD changes in both eyes; her posterior findings were otherwise unremarkable. Her preoperative CDVA was 6/9 and 6/12 in the right and left eye, respectively; her CNVA, using +2.50 DS, was N10 in both eyes. The preoperative sizes of her right and left pupils were 2.78 mm and 2.56 mm – smaller than average for her age (5) and among the smallest pupils in the cohort. Biometry suggested that an IOL power of +23.50 DS in both eyes would achieve emmetropia in the right and slight myopia in the left eye. After one month, we observed a UDVA of 6/5, UIVA of 6/6 at 60 cm, and UNVA of N5 in both eyes. The patient’s binocular UDVA was 6/5 and UNVA was N5. At six-month follow-up, the IOL was stable and well centered. This patient, who had a much smaller mesopic pupil than the first case, was very happy with her distance, intermediate, and near vision, and did not require glasses at any distance; she did experience mild dysphotopsia at night, but this was not bothersome to her.
A patient’s preoperative mesopic pupil size may be an important variable to keep in mind when considering postoperative UNVA. Patients with large pupils should be counseled regarding the possible need for postoperative reading glasses, in particular for smaller print sizes. In contrast, patients with smaller mesopic pupil sizes may experience improved near vision with EDoF IOLs, which will further enhance depth of focus. Of course, these conclusions are based on the average preoperative pupil size of our study cohort, with further data and a sufficiently powered prospective study required to confirm the extent of this relationship.
Selecting the best IOL for cataract surgery is a multifactorial decision that requires the clinician to consider the condition of the eye alongside the patient’s goals and lifestyle needs. The outcomes that can be achieved with presbyopia-correcting IOLs are influenced by the ocular surface, cornea, optical axis, disc and macula health, and endothelial cell density. Our results suggest that, in patients who opt for a premium EDoF IOL, it is also important to consider the influence of preoperative mesopic pupil size. Through good surgical planning, accurate biometry, and use of the TK formula, most patients can achieve highly satisfactory outcomes – the ultimate sign that the right choice was made (6).
Both authors have no financial interest in the products mentioned and are consultants to Carl Zeiss Meditec.
References
- MA Woodward et al., “Dissatisfaction after multifocua intraocular lens implantation,” J Cataract Refract Surg, 35, 992 (2009). PMID: 19465282.
- G Labiris et al., “A systematic review of pseudophakic monovision for presbyopia correction,” Int J Ophthalmol, 10, 992 (2017). PMID: 28730093.
- S Ganesh et al., “Clinical outcomes, contrast sensitivity, reading performance and patient satisfaction following bilateral implantation of AT LARA 829MP EDoF IOLs,” Clin Ophthalmol, 15, 4247 (2021). PMID: 34707344.
- I Hernández-López et al., “Biometry, refractive errors, and the results of cataract surgery: a large sample study,” J Ophthalmol, 2021, 9918763 (2021). PMID: 34007484.
- SJ Linke et al, “Mesopic pupil size in a refract surgery population (13,959 eyes),” Optom Vis Sci, 89, 1156 (2012). PMID: 22773178.
- P Saini et al., “To compare the refractive outcomes after cataract surgery using conventional keratometry (K) with Barrett Universal II formula and total keratometry (TK) with Barrett TK Universal II formula for intraocular lens power calculation,” Investig Ophthalmol Vis Sci, 61, 609 (2020).
