
As a second-generation ophthalmologist in a small cornea practice, I have seen corneal collagen cross-linking (CXL) evolve from an experimental procedure to an out-of-pocket service – and, finally, to a treatment covered by insurance.
Today, the majority of commercial health plans in the US – representing >95 percent of commercially covered lives – now recognize FDA-approved CXL solutions and devices as a covered service. My father and I have been offering CXL (see Figure 1) for several years and have performed more than 750 procedures to date. Today, most of my insured patients are covered and our practice is getting paid fairly – but it wasn’t always that way.
When the payment model for CXL first changed, there was a tremendous amount of confusion on the part of practices and insurance carriers about how to bill for it. We had problems with the insurance carrier classifying FDA-approved CXL as an experimental procedure (it wasn’t); paying for the Photrexa drugs but not the procedure (or vice versa); and establishing non-intuitive and often nonsensical criteria for progression.
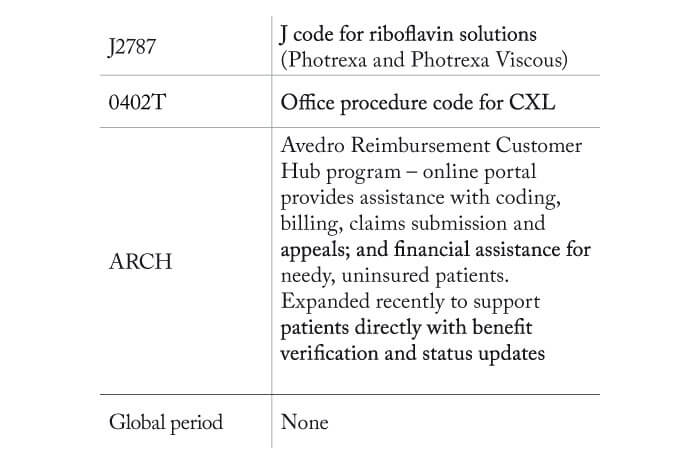
In many cases, the procedure was “covered” but not paid at a sustainable level. However, the insurance companies successfully climbed the learning curve, and so did we. We now rarely have a problem getting paid for the procedure (See box: “Billing Essentials”). Here are four lessons we learned along the way:
There is definitely a learning curve in filing insurance claims for CXL. We made the commitment to do the work ourselves, rather than ask patients to file appeals. We knew that if the system was hard for us to navigate, it was going to be doubly hard for patients. It is important to assign someone knowledgeable and persistent with the task of seeking pre-authorization, filing claims and following up on appeals and payments. It will take much longer to get claims paid if the individual with this responsibility can’t answer questions herself or himself, and needs to ask the doctor about insurance company requests.
Insurance company requirements for documenting progression may differ significantly from how a cornea specialist defines progression. In our case, the dominant carrier in our region wanted to see an increase in Kmax ≥ 1.0 D over any time period, along with a change in spherical equivalent of 1.0 D or a change in cylinder of 0.5 D. These requirements don’t make a lot of sense to me, but I have learned to accept that, regardless of how I choose to clinically define progression in examining and counseling my patients, I need to meet this coverage area for the procedure to be covered and paid.
We reached a similar conclusion with the carrier’s requirements that the patient must have “failed conservative treatment.” Given that there is no other therapeutic treatment for keratoconus, how should one demonstrate failure? My approach has been to document that the patient “failed glasses and contact lenses.” Vision correction is a conservative approach and it is reasonable to say that it has failed to stop the disease from progressing.
We learned the hard way that insurance companies wanted things to happen in a certain sequence that didn’t always make sense to us. For example, when we submit a claim for CXL for keratoconus, it routinely gets denied. The reason for the denial is “must demonstrate progression.”
Submitting evidence of progression with the initial claim did no good. The evidence for progression was only allowable (i.e. could only be submitted) after the initial rejection. So, we just adapted to the successful cadence: Submit claim; receive denial; provide evidence of progression; receive approval.
Given that many of our patients travel long distances, we have tried to set up systems that allow them to be treated them quickly – preferably on a same-day basis. We perform CXL in an exam lane with our regular technicians assisting, so that the procedure can be worked in on any regular clinic day, although we do cluster CXL procedures on Fridays when possible.
We have also educated doctors who refer to us to send us evidence of progression in advance so that we can evaluate the patient and perform CXL the same day. Those referring providers are then able to provide postoperative care in a location that is geographically more convenient for the patient. Not only does this benefit the patient, it also limits unnecessary visits for our practice.
Unfortunately, we still have two challenging categories for which insurance will not reimburse. The first is patients with post-refractive surgery ectasia. Although it is an approved indication for CXL, carriers typically consider this a complication of an elective procedure and therefore not a covered service. To me, that is regrettable, because many patients with ectasia probably had subclinical or undiagnosed keratoconus before their LASIK surgery.
The second category is patients who have a combination of Medicare and Medicaid coverage. Unfortunately, their insurance doesn’t cover or pay for CXL, so I don’t have a great solution for them. Avedro offers a patient financial assistance program which helps often – but not in all cases. Fortunately, this is a rare circumstance, as the need for CXL is uncommon in the Medicare-age population.
We are now the busiest CXL site in Alabama, with a reputation for quality care. Whether we perform CXL or not, we have proved to our patients – and their optometrists – that we can meet all their eye-care requirements, from corneal transplants to cataract surgery and glaucoma treatment. This success has come from us offering CXL; it has boosted our patient and surgical volume, solidified our reputation as providers and expanded our referral network, not just in Alabama, but in several surrounding states as well. If you are considering adding CXL to your practice, take our advice, learn from these lessons, and be prepared to reap the rewards.
