Imaging the retina to understand systemic disease is not a new concept – you’re able to noninvasively image not only the retinal vasculature, but with optic nerve and the retinal nerve fiber layer, neural tissue too. This is beginning to be exploited to map the progression of both vascular and neurological diseases (1,2). It’s also starting to be useful in predicting outcomes after patients have experienced a stroke (3).
Severe strokes tend to result in sharp increases in intracranial pressure (ICP) – and makes for a poor prognosis for the patient. ICP can be measured by lumbar puncture, but this is invasive, and can easily be confounded by other aspects of the patient’s medical management, such as acute sedative use. It turns out that measuring the optic nerve sheath diameter (ONSD) with optic ultrasonography (OUS) is a promising method of assessing ICP.
How was this established? Researchers at the Gainesville campus at the University of Florida performed OUS on patients (n=86) who presented with stroke on both the day of admission and one day later, measuring ONSD – transversely and laterally – in both eyes (3). Regression analysis was then used to assess the relationship between ONSD and patient outcomes.
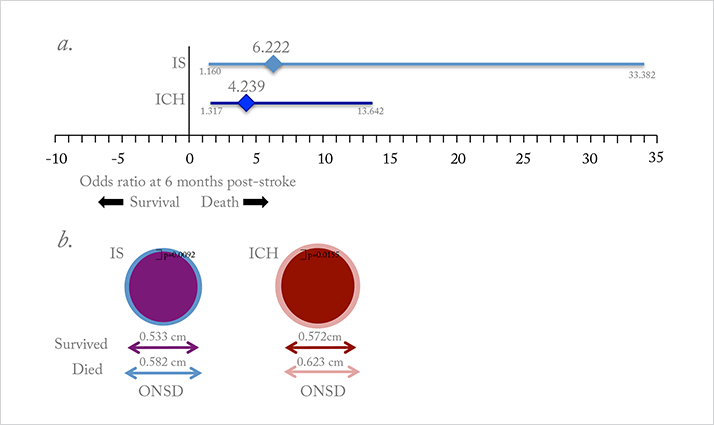
The researchers found that there was a significant difference in mean ONSD between patients who died within the first six months and those who survived: for every extra millimeter, the risk of death was four times higher in patients with ischemic stroke, and six times higher in patients with intracerebral hemorrhage (Figure 1a). Larger ONSD was also associated with a greater probability of death after six months (Figure 1b), poorer functional outcomes, and more severe disability. The authors are hopeful that OUS could offer an attractive screening alternative for ICP, as it is a routine bedside test that is performed using gel and a device placed on closed eyelids, potentially allowing doctors to reliably and noninvasively detect elevated ICP and initiate ICP-lowering treatment earlier.
References
- M Zacharria, “In the Eye of the Storm”, The Ophthalmologist, 1, 16–23 (2013). http://bit.ly/top0113. WW Lee et al., “Retinal nerve fiber layer structure abnormalities in schizophrenia and its relationship to disease state: evidence from optical coherence tomography”, Invest Ophthalmol Vis Sci, 54, 7785–7792 (2013). PMID: 24135757. VS Hedna et al., “Use of optic nerve sheath diameter in emergency department to predict stroke outcome”, Stroke, 46, Abstract: AWMP83 (2015).
