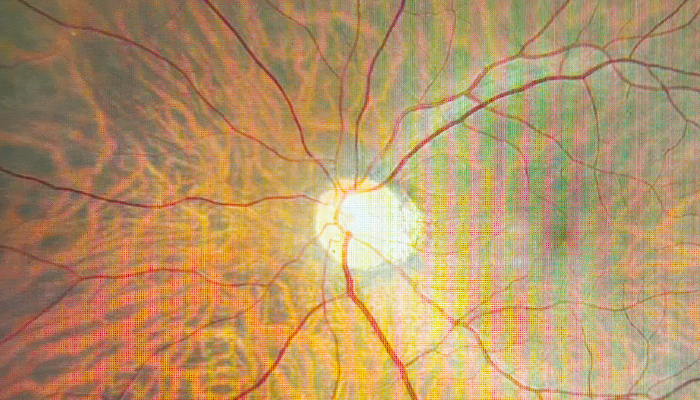
Credit: Shutterstock.com
A recent study undertaken by researchers at Columbia University Irving Medical Center has introduced a new pattern-based optical coherence tomography (OCT) metric for detecting glaucomatous damage. Developed using a logistic regression modeling (LRM) model, the novel metric leverages six variables derived from characteristic patterns of glaucomatous loss observed in OCT scans of the ganglion cell layer plus inner plexiform layer (GCL+IPL) and retinal nerve fiber layer (RNFL).
The research team, led by Donald C. Hood and colleagues, analyzed OCT data from multiple cohorts, including 400 healthy individuals and 207 with OCT-detected glaucomatous optic neuropathy (ON-G). Sensitivity and specificity were evaluated using additional test sets, ensuring a wide range of glaucomatous damage levels. Results showed that the new metric achieved a partial area under the ROC curve (AUROC) of 0.92 and a sensitivity of 88.8 percent at 95 percent specificity – significantly outperforming previous OCT metrics, such as global RNFL thickness (57.5 percent sensitivity) and global GCL+IPL thickness (47.6 percent sensitivity).
The authors believe this new metric could be particularly useful for detecting subtle patterns of glaucomatous damage that are often missed by other conventional OCT measurements. By accounting for regional vulnerabilities, such as superior and inferior arcuate thinning, the novel approach demonstrates higher accuracy for both clinical practice and glaucoma screening programs.
The authors emphasize that the new OCT metric could improve glaucoma risk assessments, aid primary care referrals to specialists, and serve as a reliable endpoint for clinical trials. They also highlight its potential role in refining OCT reports to better support clinical decision-making, bridging the gap between automated and subjective interpretations of glaucomatous damage.
