
When implementing any new technology into an established practice, the more time spent educating staff prior to roll-out with patients, the greater the chance of success. This same theory applies when it comes to building a successful dry eye practice; the whole team needs to be included in the process.
Staff members play varying but equally important roles in facilitating the right diagnosis, such as gathering critical information, helping to educate patients about ocular surface disease and the treatment options, paving the way for the doctor to have an efficient consultation, and following through on the physician’s recommendations. We know, for example, that most cataract patients have some form of ocular surface disease (1). But it is highly inefficient for the cataract surgeon to be the first person to discuss this with the patient or begin to investigate the extent to which it will affect their cataract surgery choices and outcomes. Instead, staff should play a key role in proactively gathering the diagnostic information the doctor requires.
At our practice, we start every workup with a version of the Standard Patient Evaluation of Eye Dryness (SPEED) questionnaire – with additional questions about allergy and autoimmune disease. Any positive results are then built into the patient’s chief complaint and lead to further testing.
Typically, we will image the meibomian glands using a dynamic meibomian imaging device (LipiView II, Johnson & Johnson Vision). We also test for the tear film marker MMP-9 using the Quidel InflammaDry test and for tear osmolarity using the TearLab device. We will then look at the LipiView interferometry, which measures the lipid layer thickness and can tell us whether there is a full or partial blink. During the slit lamp exam, the physician performs a diagnostic meibomian gland expression, using a Q-tip or the Korb meibomian gland evaluator. With all this information in hand, the physician can make a clear diagnosis of the type(s) of dry eye the patient has.
In addition, diagnostic testing can also help us to educate patients (see Figue 1). Meibography images can be a powerful way to show patients the difference between normal, healthy glands, and their own. A positive MMP-9 test can help us emphasize the importance of getting inflammation under control, so that patients get the best possible outcome from their investment in a premium IOL. Imaging and testing can also help to improve the patient’s engagement with their eyedrop or home hygiene regimens.
Physicians have a relatively brief time with the patient. It simply isn’t practical for everything about different treatment options to be covered in a single conversation with the surgeon – nor can we expect patients to take in all this detail and make financial decisions on the spot.
In-office procedures like LipiFlow thermal pulsation therapy have really changed the standard of care for patients with meibomian gland dysfunction. But because they are relatively new and require an out-of-pocket investment by the patient, we do need to educate patients about them – particularly, how these procedures can make a difference in their comfort, vision, and in the success of other procedures, such as LASIK or premium IOL surgery, that they may be undergoing.
A key factor in successful patient education is teaching everyone in the office to use the same terminology. By speaking to the patient with a consistent message that gets repeated over time, we can help them absorb what they need to know to make decisions. And it also keeps the lines of communication open; patients can ask any staff member a question and get an answer.
In our practice, when the patient calls to make an appointment for a dry eye evaluation, the call center staffer might say, “Well, we have a lot of new things available for dry eye right now. I’d love to have one of our counselors give you a call and talk to you about some of the treatments we offer prior to your appointment.” From my experience, patients are usually very receptive to this and are grateful for the information. If a practice already has patient counselors for refractive or cataract surgery, I’m a huge advocate of using those counselors for dry eye as well. An initial call from the counselor plants the seed with the patient about the advanced diagnostics we use, and the new treatment technologies that might be recommended for them.
When they come to the office, the technician performing the testing will be introducing dry eye concepts, and educating patients about their test results as they go through the workup. Our technicians are also trained to listen for trigger words – if the patient does mention anything unusual, the technician knows to probe for more information about which drops they are using and why the patient is using them. The answer may be an indication that the patient is using the wrong product – for example, a vasoconstrictor for redness instead of treating the chronic dry eye or allergy – and provides us with the opportunity to introduce alternative treatments or a better choice for an over-the-counter drop.
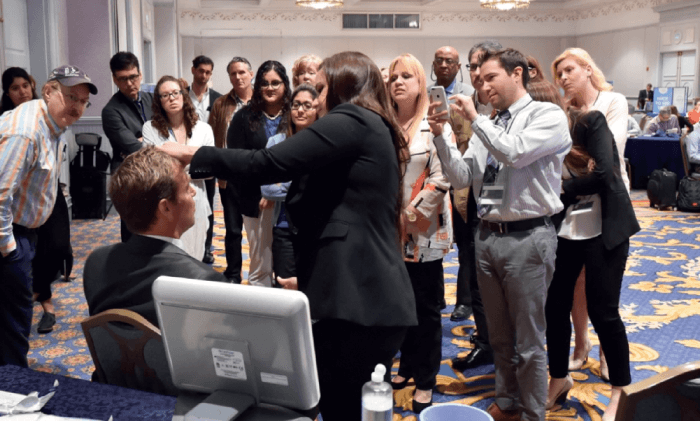
Next, the patient counselor will meet with the patient in person to continue the education process (see Figure 2). Counselors won’t diagnose a patient, but they might say, “It looks like you have signs and symptoms of dry eye, let’s review some of the available technologies that the doctor may recommend to you.” Because a diagnosis hasn’t been made at this point, nothing is certain, and our counselors are careful to communicate this to patients.
It is important that patients feel like they’re in an environment where staff members throughout the office care about their dry eye. Part of this is ensuring that they feel no symptom has been dismissed and that staff are ready to offer solutions and resources. Therefore, when the physician finally examines the patient, they are ready to hear the diagnosis and treatment recommendation without feeling overwhelmed or pressured.
I also believe physicians should make recommendations based on the standard of care for their practice, without regard for the patient’s race, gender or perceived financial status. The counselor can follow up immediately afterwards with information about Care Credit or other financing for the exact recommended treatment. If the plan involves more than one type of treatment — Blephex blepharoexfoliation and LipiFlow thermal pulsation therapy, for example — we typically bundle that into a single monthly payment for the patient.

A great benefit of getting the staff involved in patient education is that they can share their personal experiences in an authentic way. Our team members with dry eye are given the opportunity to have the treatments themselves, meaning they have first-hand knowledge – and this resonates with patients. Even those who don’t have dry eye find it easy to talk about the procedures that we do because they have seen the repeated successes with our patients.
A team-based approach, in which everyone in the practice plays a role in educating patients, is one that works not only for dry eye, but for any service where we are asking patients to make a decision that involves their financial commitment – including corneal refractive surgery, premium IOLs, MIGS devices for glaucoma, and aesthetics.
There are a number of training resources available for doctors and staff who want to get more involved in patient education. I’m obviously an advocate of the Dry Eye University program (see Figure 3) and the online Dry Eye Access platform, but there are many other resources available, such as in-person training opportunities at professional meetings or through industry, podcasts from Dry Eye Coach, and a wealth of journal articles on the topic. Any practice that wants to make a commitment to getting staff off the sidelines and participating as full members of the dry eye team has a wide range of opportunities to learn more about how to engage staff and talk to patients about this important condition.
Disclosure: Barkey has worked as a consultant for Johnson & Johnson, Allergan, Care Credit, Blephex and Alcon.
References
- WB Trattler et al., “The Prospective Health Assessment of Cataract Patinets Ocular Surface (PHACO) study: the effect of dry eye”, Clin Ophthalmol, 11, 1423 (2017).
