Corneal collagen cross-linking (CXL) is a successful, reliable and reproducible procedure with a long history already. But I do have a wish list for how I would like to improve CXL – and the good news is that clinical investigation is already well underway for many of the items on my wish list. We could start by making it more comfortable for patients than it is today.
We could improve the efficacy of the procedure by targeting specific areas of the cornea in a more customized way. And finally, we may be able to improve the reproducibility of the procedure by better mapping and treating corneal biomechanical changes, rather than just the effects of the disease. Each of these improvements builds on the previous gains.
Performing cross-linking without removing the epithelium has the potential to make the procedure both safer and less painful (1, 2). Most of the (admittedly rare) complications of CXL are related to delayed or abnormal epithelial healing (3). There have been a number of failures with transepithelial or epi-on procedures in the past. These prior attempts at epi-on CXL have largely focused on modifying the light intensity and riboflavin formulation, which are certainly necessary to success. However, the third pillar of cross-linking is corneal oxygen, which has not previously been addressed. Ongoing research in Europe and elsewhere suggests that supplemental oxygen can improve the efficacy of epi-on CXL.
Reports have shown that with the new oxygen supplementation techniques (Boost Epi-On), the demarcation line – which I consider the most reliable way to judge the extent of the treatment effect – is quite deep and similar to the demarcation line of standard, epi-off procedures (4). To me, this demonstrates that we are nearing the end of the era of de-epithelialized CXL. In my experience of performing Boost Epi-On CXL, the epithelium is unremarkable by day two. And that’s much more comfortable for patients.
Although we continue lubricants after surgery, we have been able to discontinue antibiotics on day two or three, and have switched to topical NSAIDs, without any topical steroids. The reduction in steroid use and the number of topical drops overall is another benefit of the epi-on approach. Preserving the epithelium also provides an additional 50-µm margin of safety, expanding the pool of candidates to those with thinner corneas.
Current cross-linking procedures apply light uniformly over a standard 9.0-mm zone. However, the ability to treat specifically the areas implicated in keratoconus progression, or to focus the treatment on the central 3.0 mm of the cornea that is most critical for vision, would be very helpful. Coma from an irregular cornea has a debilitating effect on visual function. Customizing the treatment profile could potentially augment the effects of CXL by creating a more normalized cornea and one with less coma.
It has been proposed that treating only the cone, rather than entire cornea, could be effective (5). Topography-guided PRK (TPRK) with CXL has been used as one way to customize this procedure, based on treating the cone directly. However, in some cases, the anterior cone is not located in the area of greatest thinning. Using TPRK may enable us to regularize the anterior cornea but could still be detrimental if there is tissue removal in the thinner areas of the cornea. What if we could use posterior elevation tomography data to treat the weakest or thinnest point of the cornea more precisely with cross-linking (without removing any corneal stroma) instead? This could increase the efficacy of the procedure without further weakening the cornea.
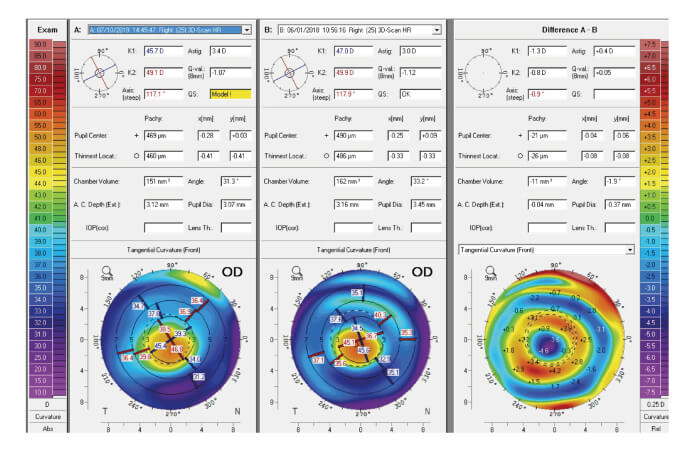
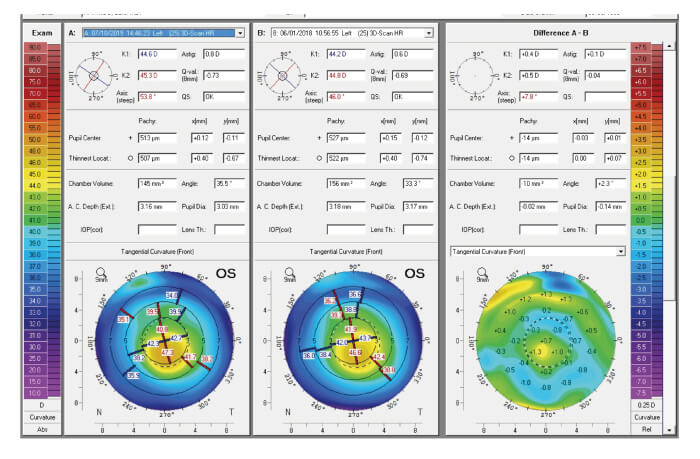
Seiler et al found that patients treated with customized irradiation patterns centered on the maximum of the posterior float had faster healing, a better regularization index, and were more likely to achieve flattening of Kmax of 2.0 D or more (6). So far, I have completed 50 cases of Customized Remodeled Vision (CuRV) with a system that combines an eye tracker with an adjustable ultraviolet light device (Mosaic, Avedro) to irradiate the cornea in a customized pattern, as determined by Pentacam tomography (Oculus). At present, we are targeting three treatment zones – each with a specific energy setting – using an epi-on procedure with supplemental oxygen. The results will be compared with those achieved with standard epi-on with oxygen.
We are already moving away from anterior surface-guided CXL toward posterior elevation-guided treatments, but I feel strongly that custom CXL is still in its infancy and that results will continue to get better, particularly as diagnostic imaging capabilities evolve. For example, future developments in anterior OCT may yield even better outcomes and point to new strategies for CXL customization. Perhaps one or two zones will prove ideal. Perhaps we will have specific nomograms that call for treatment to just one area of the cornea or require unique cross-linking agents. The potential variations are almost unlimited.
Keratoconus is a disease involving a breakdown in corneal biomechanics. Changes in corneal curvature, thickness and vision are the effects of the disease – but right now we are only able to reliably measure the effects, not the underlying pathology. It is likely that some of the variability we still see in cross-linking results may be due to variations in human corneal biomechanics; for example, there are some cases in which the demarcation line indicates a successful procedure but the degree of corneal flattening or change in Kmax are not as dramatic as might be expected.
It is my hope that in the future we will have diagnostic devices that can reliably map and measure biomechanics, enabling highly individualized CXL that can stop progression, normalize the cornea, and improve visual function. With CXL, we have a powerful tool. Just as we have seen with other ophthalmic tools, such as excimer and femtosecond lasers, the ways in which we use that tool will continue to evolve and become more sophisticated over time.
References
- S Nawaz et al., “Trans-epithelial versus conventional corneal collagen crosslinking: A randomized trial in keratoconus”, Oman J Ophthalmol, 8, 1, 9 (2015). PMID: 25709267.
- A Stojanovic et al., “Corneal collagen cross-linking with and without epithelial removal: A contralateral study with 0.5% hypotonic riboflavin solution”, Biomed Res Int, 61938 (2014). PMID: 25050368.
- P Hersh et al., “U.S. Crosslinking Study Group. United States Multicenter Clinical Trial of Corneal Collagen Crosslinking for Keratoconus Treatment”, Ophthalmology, 124, 9, 1259 (2017). PMID: 28655538.
- F Malecaze and K Pierne, “Topography-guided cross-linking”, European Society of Cataract and Refractive Surgeons meeting, Vienna, September 22, 2018.
- A Roy and W Dupps et al., “Patient-specific computational modeling of keratoconus progression and differential responses to collagen cross-linking”, Invest Ophthalmol Vis Sci, 52, 9174 (2011). PMID: 22039252.
- T Seiler et al., “Customized corneal cross-linking: One-year results”, Am J Ophthalmol, 166, 14 (2016). PMID: 26944278.
