- CLET is an effective procedure for LCSD in adults, but it has several drawbacks.
- CLET is expensive, it isn’t easily replicable, and it has shown limited effectiveness in children.
- SLET offers a lower cost and simpler alternative; it uses the eye’s environment as a natural ‘petri dish’ for limbal cell transplants.
- I overview the benefits of SLET versus CLET, and describe how to perform the surgery.
For over 10 years, I have been performing cultivated limbal epithelial transplantation (CLET) for limbal stem cell deficiency (LSCD), and have performed over 1,000 procedures. But I think that simple limbal epithelial transplantation (SLET) is a much better technique.
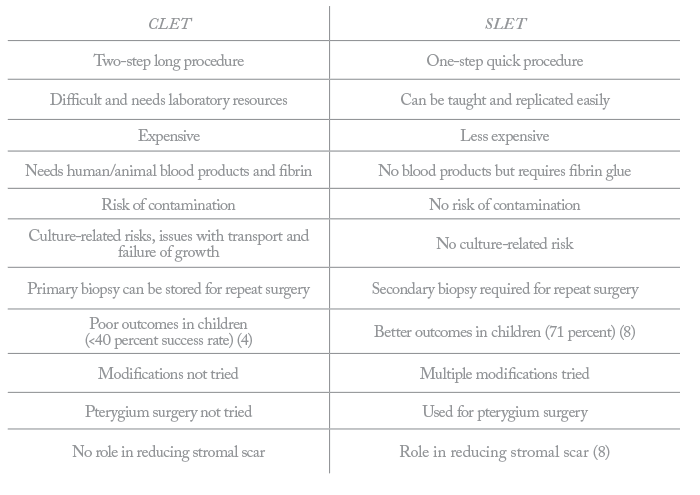
CLET versus SLET
In the CLET procedure, a limbal biopsy is harvested from the healthy eye at the first patient visit. These cells are then cultured for two weeks, before being implanted in the patient’s eye. CLET might have shown effective results (1)(2)(3), but the procedure is not a commercially-viable or scalable option. A very high quality cGMP laboratory is needed to culture the cells, which is very expensive, and there are associated regulatory hurdles. There are also logistical considerations, such as the two-week gap between the two procedures and transport of cell cultures to clinics, as well as the risks of contamination with the materials used to enable cell culture, such as fetal calf serum. Furthermore, despite 40 percent of patients needing CLET being children, the procedure is only successful in around 40 percent of pediatric cases (4).SLET is similar, but much simpler (See “Step-by-Step SLET”) – and there is a nice story as to how it evolved (See “The Evolution of SLET”). As in CLET, a limbal biopsy is taken from the healthy eye, but instead of being cultured and expanded in the laboratory, the cells are implanted onto an amniotic membrane attached to the surface of the diseased eye (5). SLET uses the environment of the eye as a natural petri dish. The cells are in their normal environment on the cornea and everything they need – serum, tears, oxygen – is present at physiological concentrations. Dr Nidhi Gupta from Shroff’s Charitable Eye Hospital, Delhi says “SLET is like a natural pregnancy and CLET is like IVF” – it’s an interesting analogy. The setup brings various benefits; it is an easier procedure than CLET, it is less costly as there is no need for a laboratory, there is no risk of contamination, and only one patient visit is required compared with the two needed for CLET (Table 1).
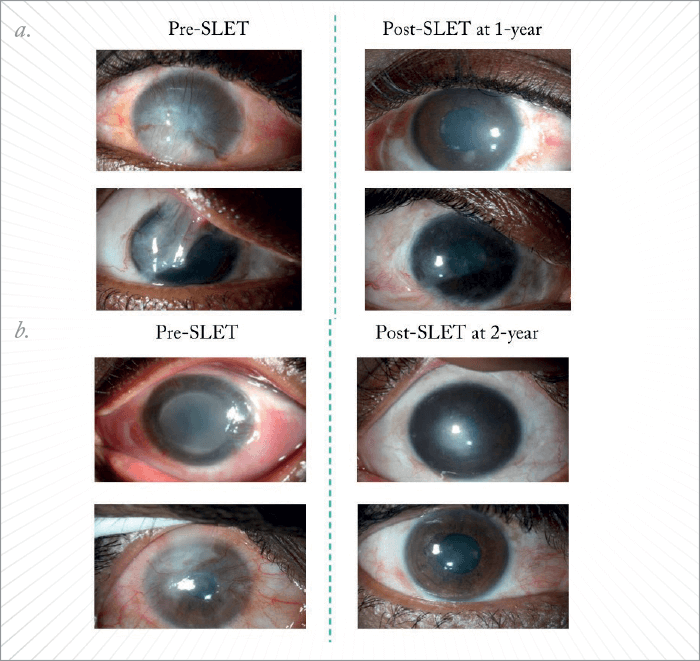
In my experience, SLET delivers excellent outcomes (Figure 1). When you observe patients over a period of time, you can see that the cornea clears – indicating modulation of corneal scarring – and that vision improves. Independent investigators have reported good outcomes with the procedure (6), and a multi-center trial across eight sites in India (Visakhapatnam, Delhi [SCEH and AIIMS], Ambala, and Kolkata), Mexico (Mexico City) and the USA (Boston and Miami) has shown good long-term outcomes with SLET (7). Furthermore, in a case series of 125 patients, we have shown that SLET was effective for long-lasting corneal regeneration, as well as being equally effective in both adults and children (8).
- Harvesting the limbal biopsy. Biopsies can be taken from the healthy eye in cases of unilateral disease, or even from a healthy area in the same eye. If disease is bilateral and extensive, lab-related or cadaveric biopsies can be obtained.
- Preparing the corneal surface for surgery. A peritomy is performed and the vascular pannus covering the cornea is excised (a–c).
- An amniotic membrane graft is placed on the ocular surface and secured in place with fibrin glue (d–f). Peripherally the amniotic membrane is tucked under the free margin of the conjunctiva (g), and the excess amniotic membrane is trimmed using Vannas scissors.
- Implanting donor tissue. The donor limbal tissue is held gently and sectioned into 8–10 small pieces with Vannas scissors, before being positioned in a circular fashion around the corneal center (h-i). The transplants are fixed in place with fibrin glue, and a soft bandage contact lens is placed on the eye at the end of the procedure (j).
Replicating success
One of the key benefits of SLET is that it is easily replicable. Even if I taught surgeons the CLET technique, there are many who wouldn’t be able to replicate it because they’d need investment from a hospital or a big organization, as well as regulatory approvals and funding for maintenance costs. CLET has EMA approval, but it costs over €50,000 to grow the cells for one patient – there aren’t many who can afford this type of treatment. It is because of this cost that I believe CLET cannot be a commercial success, although it is an academic and biological success. On the other hand, SLET is a commercial success model because minimal training is required – teaching is the only rate-limiting step. Training programs and videos are shared freely with no limitation, and there is no IP – it is an open platform technology. Rather than being possessive and attached to what I have developed, I implore people to be open and improve it – and to share their results with the community. And this has been happening – several surgeons have reported on modified SLET techniques such as Hernández-Bogantes et al. (9) on the ‘mini SLET’ procedure and Amescua et al. (10) on the ‘double sandwich’ technique. There have also been reports of using the surgery for other unique (and sometime surprising) indications, including the treatment of ocular surface squamous neoplasia (11) and pterygium (9). It is a list that just keeps growing! We have started using mesenchymal stem cells (MSCs) extensively for ocular surface disorders (12), and in the future, we are planning to investigate how we can combine SLET with MSCs to accelerate healing and expand its potential applications. For now, I feel very happy that this technique is effective, and that other surgeons are adopting it. I hope more continue to adopt this simple, yet effective, procedure. Virender Sangwan is Director of the Center for Ocular Regeneration (CORE) and Dr. Paul Dubord Chair in Cornea at the LV PRASAD EYE INSTITUTE, Hyderabad, India.The story of SLET began when Sheila MacNeil – a professor of tissue engineering at Sheffield University, UK – contacted me via email with an interest in researching limbal stem cells. In a conversation over video messaging, she had an interesting proposition: “You know Dr. Sangwan, we should have a teabag approach to the stem cell transplant,” she said. Frankly, I was unable to make the connection and told her so. But then she explained: “Right now you are growing cells in the laboratory, then transplanting them – it’s complicated. But why not approach it like tea, where people have the different components, such as milk or sugar, ready to prepare it. We can make a biosynthetic membrane with micropockets, take an explant biopsy and grow the cells on the surface of the eye.” A lightbulb went off, and that was the moment I always attribute to the genesis of SLET. Sheila said we’d need to perform some research and apply for a grant, but I didn’t want to wait. Within a week I was performing the surgery, and by the time we presented our idea to the Wellcome Trust in London, UK, I had completed five cases showing proof of the concept. Now, around five years later, the human trial of the synthetic membrane is underway, but to me, the much bigger idea is SLET. When entering that first surgery, I was a bit anxious to the extent of whether it would work or not. More than anything I felt stupid. I have probably performed the largest number of CLET procedures in the world and I couldn’t believe I hadn’t thought of this idea. But this is what comes from the collaborations you build outside of your field, and what can result from the conversations you have with others. It is so important.
References
- VS Sangwan et al., “Clinical outcomes of xeno-free autologous cultivated limbal epithelial transplantation: a 10-year study”, Br J Ophthalmol, 95, 1525–1529 (2011). PMID: 21890785. P Rama et al., “Limbal stem-cell therapy and long-term corneal regeneration”, N Engl J Med, 8, 147–155 (2010). PMID: 20573916. E Di Iorio et al., “Techniques for culture and assessment of limbal stem cell grafts”, Ocul Srf, 8, 146–153 (2010). PMID: 20712971. K Sejpal et al., “Cultivated limbal epithelial transplantation in children with ocular surface burns”, JAMA Ophthalmol, 131, 731–736 (2013). PMID: 23559315. VS Sangwan et al., “Simple limbal epithelial transplantation (SLET): a novel surgical technique for the treatment of limbal stem cell deficiency”, Br J Ophthalmol, 96, 931–934 (2012). PMID: 22328817. V Mittal et al., “Successful management of severe unilateral chemical burns in children using simple limbal epithelial transplantation (SLET)”, Br J Ophthalmol, 100, 1102–1108 (2016). PMID: 26701687. J Vazirani et al., “Autologous simple limbal epithelial transplantation for unilateral limbal stem cell deficiency: multicentre results”, Br J Ophthalmol, 100, 1416–1420 (2016). PMID: 26817481. S Basu et al., “Simple limbal epithelial transplantation: long-term clinical outcomes in 125 cases of unilateral chronic ocular surface burns”, Ophthalmology, 123, 1000–1010 (2016). PMID: 26896125. E Hernández-Bogantes et al., “Minor ipsilateral simple limbal epithelial transplantation (mini-SLET) for pterygium treatment”, Br J Ophthalmol, 99, 1598–1600 (2015). PMID: 26130669. Amescua et al., “Modified simple limbal epithelial transplantation using cryopreserved amniotic membrane for unilateral limbal stem cell deficiency”, Am J Ophthalmol, 158, 469–475 (2014). PMID: 24932987. V Mittal et al., “Primary simple limbal epithelial transplantation along with excisional biopsy in the management of extensive ocular surface squamous neoplasia”, Cornea, 35, 1650–1652 (2016). PMID: 27442321. S Basu et al., “Limbal stromal stem cell therapy for acute and chronic superficial corneal pathologies: early clinical outcomes of the Funderburgh technique”, IOVS, 58, 3371 (2017).
