- The ultimate goal of presbyopia surgery is to give patients the vision that a normal 21-year-old emmetrope has – but with current technology this isn’t possible
- Mixing and matching different IOLs makes it possible to give patients high quality vision
- Managing patient expectations is key – and the PANFOCAL visual assessment enables us to explain functional vision outcomes in a way that patients will understand
- Micromonovision is an approach to presbyopia that shows promise, and should help avoid the issues associated with traditional monovision
When performing presbyopic lens surgery, the ultimate goal is to reverse the aging effects of the eye. Ideally, we’d like to be able to provide our patients with the full range of vision of a normal 21-year-old emmetrope, so that they can effortlessly shift focus from very near to far, without spectacles, in any lighting conditions, and with each eye independently. It’s a tall task, and it’s one that we can’t achieve with current technology. But we can come close. Mixing different IOL types, or implanting an extended range of vision lens with different refractive targets, can provide almost the full range of seamless, binocular vision.
Unifying expectation and performance
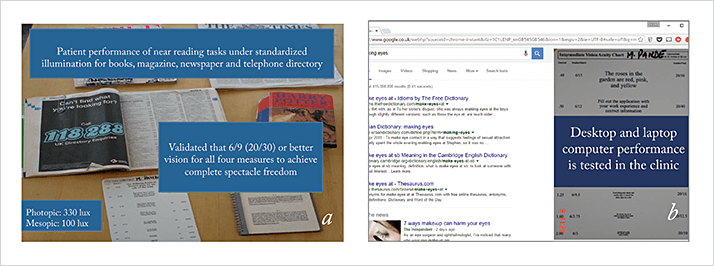
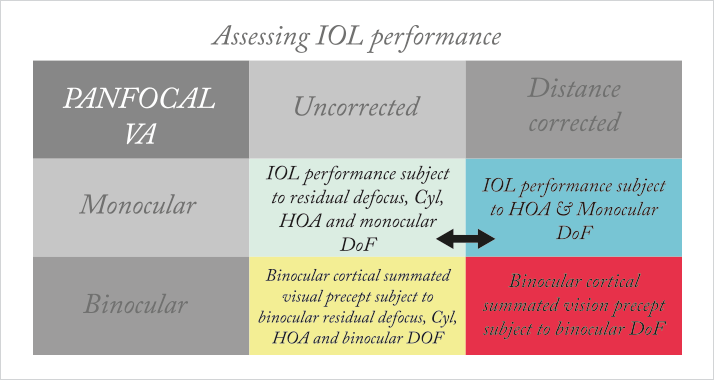
In our practice, the first step for presbyopic lens candidates is a specialized visual assessment that we call PANFOCAL visual acuity. We developed this practical clinical measure a few years ago in response to the needs of our patients, and the questions they were asking about their functional visual abilities after implantation: Will I be able to read in bed at night? To use spreadsheets on my laptop? To see the navigation system on my boat?I couldn’t answer these questions, nor could I confidently correlate real-world tasks with the acuity level necessary to perform the task comfortably, without glasses. I was concerned that this mismatch between expectations and performance could lead to unhappy patients. Measuring acuity at many points, from near to far, would be helpful… but also impractical in a busy clinic. Our solution was to conduct extensive testing in order to correlate tasks to acuity, and determine which acuity measures would be the most useful. So we asked our patients to read a variety of materials, from glossy magazines and fine-print telephone directories to a book or computer screen, in various lighting conditions (See Figure 1a and 1b).
We found that 6/9 (20/30) or better vision at four measurement points (See Table 1 and Figure 2) is consistent with successfully performing a wide range of tasks with complete spectacle freedom. Now, we routinely perform a PANFOCAL assessment at baseline, after the first eye surgery, and after both eyes have been operated on, and enter all the results into our patient database. By querying the database for any given IOL, it has been relatively easy to establish what each lens is capable of, and reliably explain it to patients in functional terms that they can understand – for example, I can tell a patient, “With lens A, 90 percent of patients can read a fine-print telephone book in bright light, but not in dim light.” The PANFOCAL assessment has also made it possible to choose two different lenses with complementary results, or choose refractive targets in order to get the patient to the ideal visual acuity of 6/9 that I know they need to be truly spectacle independent.
Mix-and-match
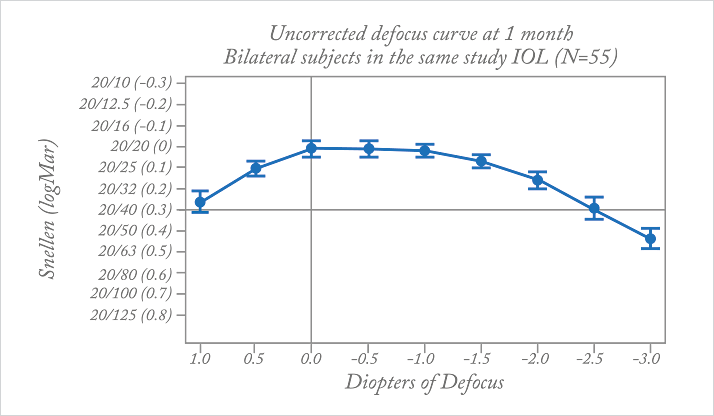
I have used a mix-and-match approach for years, combining two different multifocal IOLs (mIOLs), a multifocal and an accommodating lens, or a monofocal and multifocal. I have also performed refractive lens exchange in the nondominant eye of near-emmetropic presbyopes to give them “mono multivision”: one emmetropic phakic eye and a multifocal in the other eye. With all of the great IOLs we have available to us, selecting a mix that allows me to balance the strengths of each lens and minimize disadvantages to get closer to spectacle independence just makes sense. With this approach, I have many highly satisfied mIOL patients, but two challenges remain. Firstly, the weakest vision with any mIOL is always intermediate – a range that patients increasingly value. Secondly, there is always a tradeoff in contrast sensitivity, glare, and haloes with mIOLs. Although most patients adapt to these tradeoffs easily, minimizing these would be a significant advantage.More recently I’ve been using a new category of presbyopia-correcting IOLs, the Tecnis Symfony extended range of vision. Initially, I used it in combination with a customized choice of Tecnis multifocal lenses. The Symfony is unique in that it uses an echelette design to provide an extended range of focus, and also corrects for chromatic and spherical aberration. This optical design allows it to provide continuous vision across a range of distances (as seen in the defocus curve in Figure 3). Optical bench studies show that the modulation transfer function (MTF) curve or optical performance is similar to that of a Tecnis monofocal IOL (1), minimizing the compromises to quality of vision that we’ve become accustomed to with mIOLs. My patients report that their vision feels very natural and seamless, without any gaps in their range of vision.
Experiments in micromonovision
Some patients find that the extended range of vision lens doesn’t provide as much near vision as they would like. So, in addition to combining it with a multifocal, I’ve been experimenting with a micromonovision system.By setting the refractive target for the nondominant eye to just -0.50 to -0.75 D, we are able to fill that near gap, with excellent results – as others have also found (Figure 4). With micromonovision, the difference between the two eyes is less than 0.75 D. This is so small that it’s within the range of difference seen in the normal population. Micromonovision is not associated with the issues of traditional monovision: adaptation isn’t an issue, a contact lens trial isn’t required, and eye dominance isn’t a problem. If needed, it can be instantly reversed with glasses – something that isn’t possible if an mIOL has been implanted. It also means the patient is left with very good distance acuity, that can meet the driving standard not only with both eyes open, but with each eye individually.
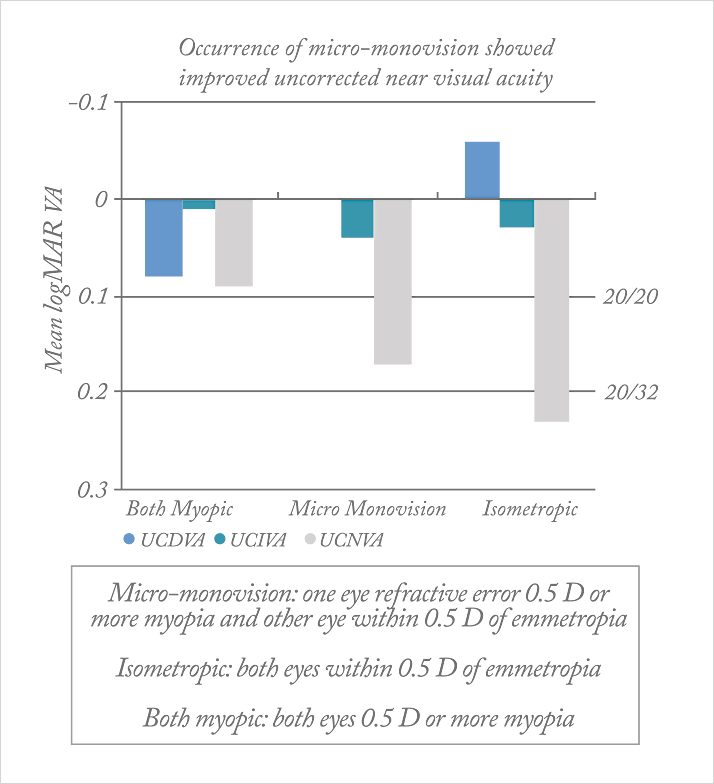
My approach is to operate on the dominant eye first, with a target of emmetropia. Many eyes have an intrinsic level of pseudoaccommodation – perhaps from pupil constriction or enhanced depth of focus due to corneal aberrations – but it is impossible to predict this preoperatively. If the patient is happy with their reading vision after the first eye, we target the other eye for emmetropia, too. But if the patients would like better reading vision, we opt for a slightly myopic target in the second eye. Our patients with micromonovision are consistently achieving 6/9 or better PANFOCAL acuity, and are spectacle-free for all the tasks that matter to them. By communicating well with patients and managing their expectations, and by utilizing the advantages of the IOLs available to us, we have been able to move closer to the ideal presbyopia correction we aim for.
Milind Pande is consultant ophthalmic surgeon and Medical Director of the Vision Surgery and Research Centre in East Yorkshire, UK.
References
- 166, Data on File, Abbott Medical Optics. Extended Range of Vision IOL 3-Month Study Results (NZ).
