Age-related macular degeneration (AMD) is the most prevalent cause of blindness of the elderly in the developed world, and the search for new and better therapeutic interventions is the subject of intense research. Despite these efforts, researchers still don’t fully understand how the disease advances. It’s known that choroidal neovascularization (CNV) goes hand-in-hand with advanced disease, and it is also thought that inflammation might also play a role in driving AMD pathology. And though treatment with VEGF inhibitors blocks the process of vascular growth and leakage, they do not lead to complete regression of abnormal vessels, and they largely ignore the role of immune cells. A team from the Massachusetts Eye and Ear Institute may have found a way to target both aspects that drive the pathology: via a subset of bioactive molecules that can resolve CNV by modulating inflammation. Kip Connor, corresponding author on the associated paper (1), tells us more about their work.
What inspired this research?
We wanted to perform this research because identifying additional mechanisms that regulate abnormal blood vessel growth in the eye could open a range of possibilities for new research and treatments for AMD.What were your key findings?
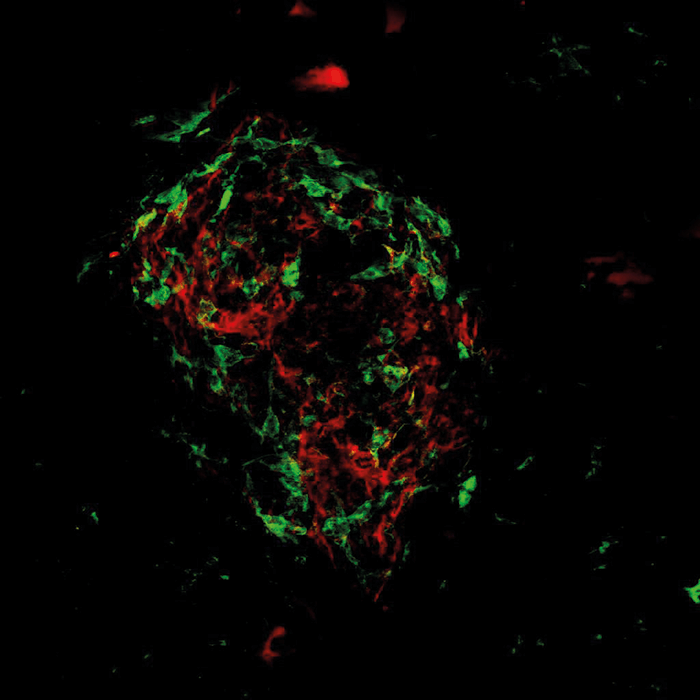
In the present study, we demonstrated that specific bioactive products from the cytochrome P450 (CYP) pathway, a major family of enzymes, could reduce the development of CNV and vascular leakage by altering how immune cells were recruited to areas of disease and injury. Specifically, we isolated and characterized two key mediators of disease resolution from the CYP pathway: 17,18-epoxyeicosatetraenoic acid (17,18-EEQ) and 19,20-epoxydocosapentaenoic acid (19,20-EDP). These bioactive metabolites reduced disease severity in a mouse model of neovascular AMD.Did you encounter any hurdles?
There are always obstacles (other than funding) that come up in research! We initially struggled to identify whether the bioactive lipids exerted their effects locally in the retina or systemically. It turned out to be a little of both: they modulated the damaged vasculature at the site of injury as well as systemic inflammatory immune cells. Such challenges make our jobs so exciting and rewarding because they really make us think about the science and push us into new areas that we may have overlooked before. I am very fortunate to be part of an amazing team, and together we overcame the challenges encountered along the way.Did you have any surprising results?
I was surprised at the degree by which systemic immune cells were affected by these bioactive lipids and the extent of their contribution on the local retinal lesions. I had imagined it would be a more focal effect.What impact do you hope your research will have?
Our study offers new insights into bioactive lipid metabolites as regulators of systemic inflammatory immune cells and mediators in CNV resolution, and it also shows the promising therapeutic potential of these bioactive products for neovascular AMD – as well as other major conditions that involve angiogenesis and inflammation, such as atherosclerotic disease and cancer. Given the high prevalence and progressive nature of neovascular eye disease, the ability to stabilize bioactive lipids that mitigate or halt disease is of great and increasing therapeutic significance. We hope that emerging technologies and future studies will expand on our work and ultimately lead to safe, targeted, and cost-effective therapies that markedly improve visual outcomes and quality of life for patients suffering from these debilitating ocular diseases.References
- E Hasegawa et al., “Cytochrome P450 monooxygenase lipid metabolites are significant second messengers in the resolution of choroidal neovascularization”, Proc Natl Acad Sci USA, [Epub ahead of print], (2017). PMID: 28827330.
