
There are a lot of safety and efficacy data available for excisional goniotomy with the Kahook Dual Blade (KDB). How does it reflect your real-world experience?
Paul Singh, MD: The results from both within our practice and in the published literature marry together nicely – with an average reduction in intraocular pressure (IOP) being around 30 percent, and medication taken by patients reduced by more than 50 percent (1). The published research has shown that excisional goniotomy with the KDB is consistent and repeatable, whilst retaining high levels of safety. In the majority of eyes diagnosed with open angle glaucoma, we find that the resistance to outflow is at the level of the trabecular meshwork (TM) – so, by removing that diseased tissue, we have direct access to the canal and distal collector channels. Using KDB creates a very clean excision, which you can see even at an electron microscopy level – the cut is a little bit cleaner compared with other devices, which is great for the surgeon and the patient. Using the KDB is very intuitive, with clear visibility of the canal of Schlemm anterior wall – this means there’s a very clear endpoint and clear verification that you have excised the TM during the procedure. With other procedures, surgeons don’t get such a clear-cut validation that they’ve done the right thing, or that they’ve actually made an improvement in outflow – but with this tool, you have that confirmation.

What were your impressions of the KDB, and how does the new KDB GLIDE® compare?
Michael Greenwood, MD: I enjoyed the simplicity of the original KDB and not having to worry about an implant, which increases the procedure’s safety and efficacy, and reduces dependency on the implant being in the right spot.
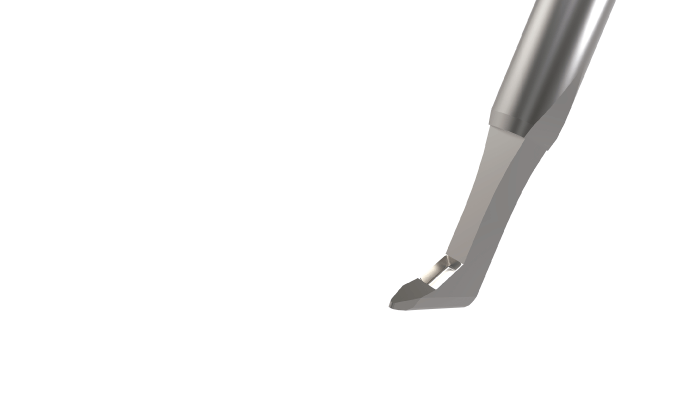
However, what surgeons sometimes found was that if they pushed in a little bit too hard, the KDB would get stuck on the back wall of the canal of Schlemm, potentially causing some ocular torsion. The subtle changes that resulted in the KDB GLIDE® have allowed it to do exactly what the name suggests: it glides through the canal and TM a little bit smoother. It’s an upgrade, with improvements that on the surface probably don’t seem huge, but they allow the end product to easily move through the tissue.
The thing that I really like about both these instruments is the dual blade, which means that as you’re moving through the TM, it’s cutting as wide as it can. Instead of making a single slice through it, it makes two parallel incisions and allows me to physically remove that meshwork, whilst giving the widest cut and the greatest chance of success with it.
It was great for me to try out the KDB GLIDE® early, in a wet lab situation, and I was able to give my feedback at that stage – it was a “thumbs up” for a job well done in producing a product with a noticeable difference. It has made goniotomy even easier.

Singh: I actually wrote a song about it called “GLIDE!” You can guess what has improved from the name alone. The KDB was already smooth to work with, but what New World Medical achieved with the new version is to make it even smoother, so that it basically glides through the TM. To be more specific, they rounded the heel, tapered the sides of the device and the blades, and made a smaller footplate – this still allows engagement with the TM, but also enables a smooth glide through to the canal. The tapered sides and rounded heel ensure it doesn’t get hung up or stuck, which was something that could happen against the canal of Schlemm before – not the end of the world, but you would have to re-engage and hit some resistance. The KDB GLIDE® allows the surgeon to smoothly excise the TM with less resistance than the original KDB and has the additional advantage of a slightly smaller footprint, allowing better angles and making the process easier for smaller canals that would have been trickier with the previous version. Notably, the width of the ramp and distance between the blades has not changed, thus still resulting in almost complete excision of the TM with every treatment.
With KDB GLIDE®, there’s minimal manipulation of adjacent tissues, although you are excising the diseased TM tissue. It is user friendly for the surgeon, with an ergonomic design to the handle and the weighting of the device, and it lends itself to an efficient procedure. I think that because surgeons are comfortable in different positions when working, the flexibility of direction and maneuverability with which this product allows them to excise the TM is ideal. Whether they prefer the outside in, or inside out technique, there’s a comfortable way to excise the TM for any surgeon by varying their view, hand position, and how they’re sitting. So, to summarize, it’s efficient, user friendly, and enables clean verification, and clean excision of diseased tissue. It really is a common-sense piece of equipment, and one of the most efficient, intuitive, products to perform excisional goniotomy.
Which patients is the tool most useful for?
Greenwood: The beauty of the KDB GLIDE® and goniotomy in general is that it can be applied to almost any patient type. In our practice we’re using it on patients with advanced glaucoma without concomitant cataract surgery or those suffering from cataracts who also have mild to moderate glaucoma… We’ve used it as a standalone procedure, and with phakic and pseudo phakic patients. We often use it in combination with cataract surgery to achieve both IOP lowering as well as decreasing dependence on IOP lowering medications.
The other nice thing about KDB GLIDE® and other angle procedures is that you can pair them with other minimally invasive glaucoma surgery (MIGS) devices. Often my pseudo phakic patients come in because they have advancing glaucoma, and they either need more medications or they’re on too many medications already. If I can do KDB GLIDE® and then pair it with something like endoscopic cyclophotocoagulation, I have accomplished two different ways to lower IOP in a synergistic manner.
Singh: It’s great for those patients who are prone to issues with compliance, even if they’re controlled from an IOP perspective – for example, those who are pseudo-phakic and are on a number of medications. I think the impact of compliance shouldn’t be ignored, whether it’s due to ocular surface disease, forgetfulness, adverse events with the drops, hyperemia or cost. There are so many different reasons why patients just cannot take their medication.
I also use it for patients with complicated histories like combined mechanism glaucoma – post LPI, where angles are open, but the IOP is still not controlled. This is where I love using KDB, because the disease in that condition is within the unhealthy TM, and it’s so satisfying to be able to remove it. For patients with a history of peripheral anterior synechiae (PAS), or secondary glaucoma with PAS and scarring, I use the KDB to remove scar tissue, pull it back away from the PAS and excise the unhealthy TM. The device is great in those situations.
There is also a clear role when KDB is combined with cataract surgery in patients with open angle glaucoma, who are on three or four medications. As long as you have an open angle, and a good view of the TM, this technology is a good option.
I won’t use this for younger phakic patients who are on one or two medications for mild glaucoma – this is because I want to hold off on removing TM right away, sparing as much for later as possible. There are some patients where I’ll use it to help at the time of cataract surgery, but I’ll find myself using it a lot more in patients where I go back to perform a MIGS standalone, as it’s effective and efficient.
How are your KDB GLIDE® patient outcomes?
Singh: I have seen a number of patients with failed trabeculectomies, for whom I was able to use the KDB to help revitalize the conventional pathway by opening up the TM. Having this option for mild, moderate, and advanced glaucoma patients, and any number of medications, is ideal, and is one of the major advantages of the KDB – giving me the flexible opportunity to help improve patients’ quality of life and reduce their IOP.
Greenwood: In my experience, patients are happy with outcomes, and so are the clinic staff. We’ve had success in lowering patients’ medication burden, getting them off at least one medication. Of course, the result is more dramatic in patients with IOP around 30 mmHg, which we are able to halve, rather than a patient with the IOP in the mid-teens, which we can lower by a couple of points.
What would you say to a surgeon who is yet to use the KDB GLIDE®?
Greenwood: The KDB GLIDE® is very straightforward and intuitive to use – surgeons can efficiently move the device in the canal and along the TM. The device is so simple yet versatile that you can perform the procedure forehand or backhand, and it doesn’t matter if you’re right- or left-handed. You don’t have to worry about placing an implant, so if you’re new to MIGS or just getting started in your practice then this is a great instrument to start with – as you’re just removing the diseased TM and don’t have to worry about the placement or losing the device.
The simplicity of the KDB GLIDE® is what I really like about it – once you’ve got a view of the TM, you gently place the device, move it along the canal of Schlemm, and it leaves this nice ribbon of tissue that you can either remove or, alternatively, allow it to scroll and ball up locally without needing to remove it.
Singh: It’s a great option – as MIGS surgeons we have to stay on top and adapt to different products and devices. There are no perfect solutions or products – they all have their specific benefits. The KDB GLIDE® is a device that really makes the surgeon feel comfortable with excising the TM. Yes, stenting is a good option for some patients, and viscodilating is good for others, but adding excision of the TM as a string to your bow is a great benefit – especially when you consider that most, if not all, patients’ disease is primarily located in the TM, and the only way to get that outflow facility is to remove the TM.
I think it’s good to start with the KDB GLIDE® as the learning curve is fairly quick and it’s a very intuitive piece of equipment, so teething problems aren’t really an issue. As long as you have a good view of the angle, it is a clean and efficient surgery. How much of the TM or how much of the angle to excise is a common question, but you don’t have to do more than ~90 degrees (3-4 clock hours) to achieve significant outflow improvement. I excise whatever I can see with the gonioscopic viewer because even from that I have found access to two or three collector channels. Of course, the more experience you have with different techniques, the greater your perspective on what is necessary in a particular case.
Let’s not forget the impact and importance of removing the number of drops that a patient has in their regimen – we define MIGS success in terms of IOP lowering, but it can’t just be classified as a reduction of pressure, it also comprises the reduction of medication burden. We have worked out that by just removing one drop from a patient’s regimen, we can save four minutes per patient visit per technician. By addressing and intervening with glaucoma as early as possible, and managing compliance issues, we can save a lot of time. It is also a surefire way to make a surgeon popular with their staff, who love it when we get people off drops, as they are the ones spending more time than us verifying, checking, making sure that generic versus brand name switches are ok – all of which adds up for the patient, but also adds lots of time for the technicians doing follow ups.

Could you share any pearls for surgeons using the KDB GLIDE®?
Singh: Just like with any other MIGS procedure, it’s really important to start out with a pristine view of the angle. Taking your time and setting up with an unfussed view with the TM perpendicular to you is critical to a good surgery – the more perpendicular it is, the better the KDB footplate will rest in the canal.
Another key point is to not point the tip towards the TM. I engage almost parallel to the TM, and I push straight back towards the angle, and glide. This is because the tip of it has a ramp which will lift the TM, gliding, cutting and excising for you at the same time – so there is no need to try and lift the TM or engage at an angle, as the ramp and the design of the blade do all the work for you. Where doctors run into problems is when they try to poke at the TM or point the tip towards it to engage and lift it, which will meet with resistance and more manipulation. What you need to remember is to let the blade do the job it was designed for.
Finally, develop a technique that you are comfortable with – Out and In, In and Out, Mark and Meet; there are different ways of removing the TM and there will be one that you are most comfortable with. For doctors that aren’t comfortable with removing TM, it’s worth leaving it until the end of the procedure. If the TM is difficult to remove and you don’t want to risk going back in and out, then it can actually be left there with no difference in fibrosis, inflammation or alignment.
Greenwood: If you’ve used the original KDB in the past and haven’t had a chance to use the KDB GLIDE®, I definitely think it’s worth making the change. The new version just glides through the TM a little bit easier and that makes the procedure a little bit smoother for both you and the patient. Making sure you’ve got a good view is key, and with the KDB GLIDE® you know if you’re too shallow with your initial placement as you just won’t remove any of the TM, which is very easy to see. Pushing too hard will cause some striae in the cornea and change your view, and that’s when you’re really going to put some torque on the eye. Just learning how to place the tip and then slide it along the TM is one of the key aspects to any MIGS procedure, but the updated design of the KDB GLIDE® makes it more forgiving, so if you are pushing a little bit too hard it still glides through quite well, compared to the original version.
References
- A Al Habash, A Albuainain, “Long term outcome of combined phacoemulsification and excisional goniotomy with the Kahook Dual Blade in different subtypes of glaucoma,” Sci Rep, 11, 10660 (2021). PMID: 34021228.
