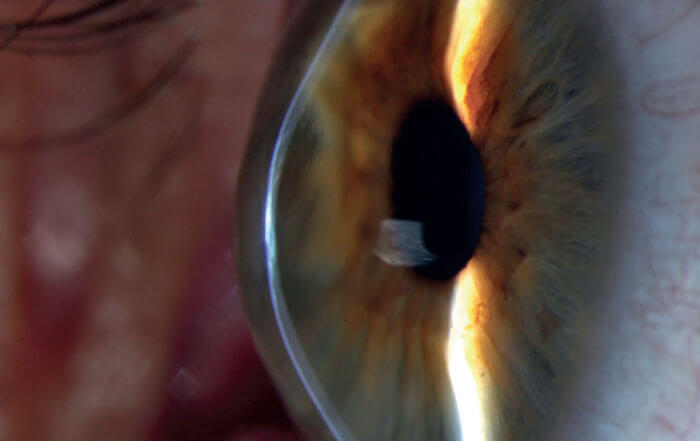
Clinicians on the lookout for keratoconus are about to benefit from a new addition to their armamentarium; Avellino Labs is developing a diagnostic genetic test for keratoconus risk factors.
Avellino’s novel technology will not only offer ophthalmologists a tool for the early detection of patients at risk of developing keratoconus, but it will also provide additional data for patients who may not be showing the classic signs associated with keratoconus when examined using current scanning technology and algorithms.
Edward Holland, Director of Cornea Services at Cincinnati Eye Institute and Professor of Ophthalmology at the University of Cincinnati, says, “Adding genetic testing to our existing optical and scanning methods will result in the ability to identify patients at risk of keratoconus earlier, perhaps before there are any changes that can even be detected on current devices.”
So how does the genetic test work? First of all, a swab is used to collect DNA from the patient’s cheek. The sample is then sent to Avellino’s lab for next-generation sequencing (NGS) and analysis. The NGS custom panel targets over 1,000 variants across 75 genes for keratoconus (KC) and over 70 TGFBI mutations for corneal dystrophies (CD). Sequence results are aligned to the Genome Reference Human Build 37, and a relative risk (RR) score is calculated for the detected keratoconus variant. Risk scores were derived from a Bayesian logistic regression model constructed from NGS results, including whole exome sequencing and targeted sequencing platforms.
Current corneal cross-linking treatments are unable to reverse the damage caused by keratoconus – and changes to the cornea can result in vision deterioration, meaning that early detection of keratoconus is a serious need. For surgery candidates, early diagnosis of keratoconus is extremely important, as it can prevent post-surgery pathology progression. Holland explains: “By identifying those at-risk patients earlier, we can improve the monitoring for younger patients and potentially implement preventative treatments, such as collagen cross-linking. Genetic testing will also allow us to have additional information in the evaluation of refractive surgery patients. Knowing a patient’s potential to progress to keratoconus could be a deciding factor in choosing one refractive procedure over another – or possibly not recommending corneal refractive surgery.”