- Many options are now available for the treatment of corneal ectasia, including intrastromal corneal ring segments (ICRS)
- Numerous clinical studies have shown that ICRS restore contact lens tolerance, improve visual acuity and may delay or eliminate the need for corneal transplantation
- A study conducted in my clinic showed that Keraring ICRS reduce corneal asphericity and keratometric astigmatism
- ICRS have a long track record of use for various corneal applications and typically demonstrate a good safety profile along with their visual improvements
Corneal ectatic disorders – like keratoconus, pellucid marginal degeneration (PMD) and iatrogenic post-LASIK ectasia – are principally characterized by a biomechanically unstable cornea. Thinning occurs in the central, paracentral, or peripheral cornea, leading to corneal steepening that commonly results in visual disturbances and poor best-corrected visual acuity (BCVA) (1). As little as 15 years ago, such patients were typically offered rigid contact lenses to “smooth” the surface of the cornea and improve their visual acuity. But when those lenses failed or became intolerable, corneal transplantation was really the only option left. The optical outcomes after corneal transplantation were generally very good, but procedures like penetrating keratoplasty are associated with a number of ocular adverse events too, like accelerated cataract development, microbial keratitis and glaucoma (2,3).
Fortunately, today’s patients have a number of alternative treatment options available to them: corneal collagen cross-linking with riboflavin and ultraviolet light, toric phakic intraocular lenses (pIOLs), simultaneous topography-guided photorefractive keratectomy (PRK), and intrastromal corneal ring segments (ICRS) – all of which can be used alone or in combination, depending on the severity of the condition.
The evolving role of ICRS
Of all of these treatment options, the one I find most interesting to use is ICRS. It may be surprising to some to learn that the use of intracorneal implants dates back to the 1950s, when José Ignacio Barraquer first proposed their use for refractive purposes (4,5). The biggest leap in the development of ICRS came in the early 1990s, when Guimarães and Nosé investigated the use of one-piece polymethylmethacrylate (PMMA) ring implants for the treatment of myopia. These corneal inserts first received regulatory approval for the treatment of myopia – in Europe in 1996 and then in the United States in 1999. Attention has turned toward their use in the treatment of keratoconus. This is hardly surprising – numerous clinical studies have shown that ICRS, which exert an “arc-shortening effect,” help to stabilize keratoconus progression and improve corneal surface regularity. As a result, they may help to restore contact lens tolerance, improve visual acuity and delay or even eliminate the need for corneal transplantation (6–9).The tailored approach with Keraring
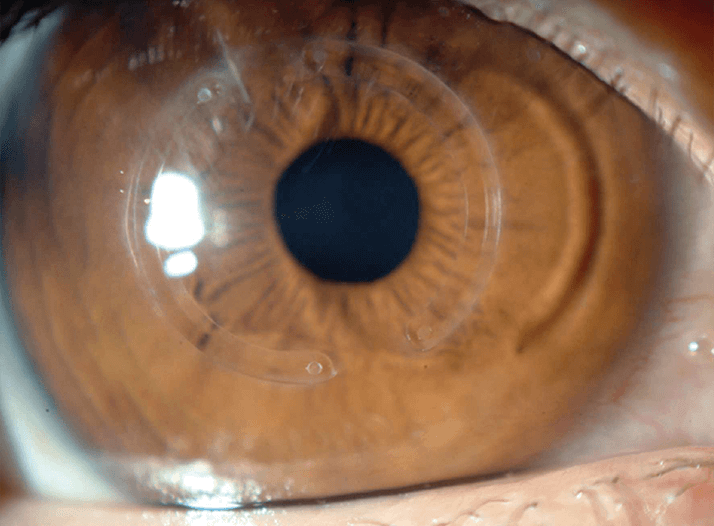
There are several commercially available ICRS, including the Intacs (Addition Technology Inc., Lombard, IL, USA) and Ferrara (Ferrara Ophthalmics, Belo Horizonte, Brazil) ring, both of which vary according to arc length, thickness, and zone of implantation (6). At my center, I use the Keraring (Mediphacos, Belo Horizonte, Brazil; Figure 1), which is available in two models – the SI5, which has a 5 mm optical zone, and the SI6, with optical zones of 5.5 and 6.0 mm. Both the SI5 and the SI6 can be used in patients with keratoconus, post-LASIK ectasia, PMD and other corneal irregularities. Importantly, the Keraring, which is composed of medical-grade polymethylmethacrylate, is available in several thicknesses (from 150 µm to 350 µm, in 50 μm increments) and arc lengths (90°, 120°, 150°, 160°, 210°, 340° and 355°), allowing these ICRS to be customized according to each patient’s needs. Keraring ICRS implantation can also be combined with other treatments for corneal ectasia such as collagen crosslinking, toric pIOLs, or topo-guided PRK (10).My clinical experience
My center, the Instituto de Olhos in Rio de Janeiro, Brazil, conducted a one-year study to evaluate the safety and efficacy of Keraring implantation in patients with corneal ectatic disease. It was a retrospective study that included 24 eyes of 18 patients (average age 19.2 years; range 18.3 to 42.0 years) whose uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), manifest refraction and corneal topography was assessed at baseline and again one year after Keraring implantation. Although many ophthalmic surgeons still implant ICRS using manual dissection, we used a femtosecond laser (IntraLase iFS [150 kHz], Abbott Medical Optics, Santa Ana, CA, USA) for our channel creation. The femtosecond laser helps us to ensure accurate centration and delivers energy to a precise depth (Figure 2). It also reduces our procedure time, thus increasing patient comfort, and may help to lessen the risk of inflammation or infection.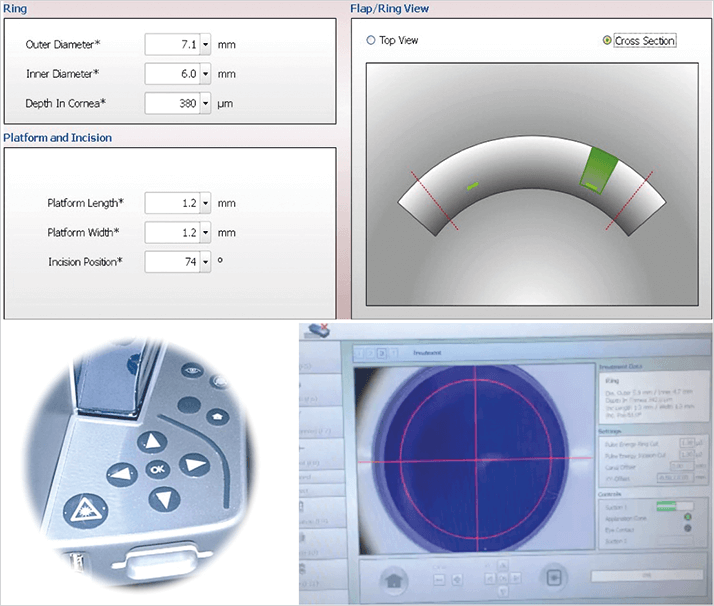
One year after ICRS implantation, we noted a statistically significant improvement in (logMAR) UDVA – for instance, one patient’s vision went from 1.25 [20/400] preoperatively ±0.48 to 0.75 [20/100] ±0.44 postoperatively, p=0.0004. There was also an improvement in CDVA, from 0.39 [20/50] ±0.25 preoperatively to 0.20 [20/30] ±0.14 one year postoperatively (p<0.0001) and a reduction in mean spherical equivalent from -6.34 ± -6.36 to -4.76 ± 4.23 (p=0.0093). Additionally, at follow-up, we found that patients’ corneas were less prolate (less negative aspherical Q front 30° values), as well as reductions in K2, front and back elevation values at the thinnest point (best-fit sphere for 8 mm), keratometric astigmatism, and maximal keratometry readings (p<0.05). Keraring ICRS have an extensive track record of use and have been evaluated in numerous studies, ranging from large randomized trials to smaller case studies using both manual and femtosecond laser techniques for channel creation. Although published studies describing outcomes with femtosecond laser-assisted Keraring ICRS implantation are somewhat limited, our data echo a one-year retrospective 50-eye study published in the American Journal of Ophthalmology in 2008. As in our study, Efekan Coskunseven and his colleagues noted improvements in UDVA and a reduction in mean spherical equivalent one year after Keraring insertion (11). Data from a six-month study of 10 patients (12 eyes) with clinically and topographically verified keratoconus performed in Istanbul, Turkey, demonstrated that Keraring insertion resulted in statistically significant improvements in BCVA, uncorrected visual acuity and mean spherical equivalence (12). In both studies, no complications occurred during either femtosecond laser or ICRS implantation, nor were any late postoperative complications observed during follow-up. These studies suggest that femtosecond-assisted Keraring implantation can provide a safe and effective method for the correction of corneal ectatic disorders.
There are refractive benefits too
Overall, our findings suggest that ICRS have a definite role to play in the treatment of corneal ectasias, and that femtosecond laser-assisted Keraring implantation appears to have a good safety profile. While the aim of ICRS implantation in patients with corneal ectatic disease is therapeutic and not refractive per se, these data indicate that ICRS implantation not only regularizes the surface of the cornea, but also significantly improves visual and refractive outcomes.Renato Ambrósio Jr. is an ophthalmologist in practice at the Instituto de Olhos Renato Ambrósio in Rio de Janeiro, Brazil. He has over 350 publications, over 50 awards in Brazil and internationally, and as a major contributor to corneal imaging technology, has helped to establish the true nature of many corneal pathologies.
References
- American Academy of Ophthalmology, “Corneal ectatic disorders (keratoconus and pellucid marginal degeneration)”, The Ophthalmic News & Education Network, (2014). http://bit.ly/AAOTONEN, accessed December 12, 2014. L. Lim, K. Pesudovs, D.J. Coster, “Penetrating keratoplasty for keratoconus: visual outcome and success”, Ophthalmology, 107, 1125–1131, (2000). I. Rahman, F. Carley, C. Hillarby, et al.,“Penetrating keratoplasty: indications, outcomes, and complications”, Eye, 23, 1288–1294, (2009). doi: 10.1038/eye.2008.305. J.I. Barraquer, “Cirurgia Refractiva de La Cornea Instituto Barraquer de America – Bogotá – Tomo I”, (1989). J.I. Barraquer, “Modification of refraction by means of intracorneal inclusion”, Int. Ophth. Clin. 6, 53, (1966). A.M. Gharaibeh, S.M. Muhsen, I.B. AbuKhader, et al., “KeraRing intrastromal corneal ring segments for correction of keratoconus”, Cornea, 31, 115–120, (2012). doi: 10.1097/ICO.0b013e3182215a15. J. Colin, B. Cochener, G. Savary, et al.,“Correcting keratoconus with intracorneal rings”, J. Cataract Refract. Surg., 26, 1117–1122, (2000). Z. Tunc, F. Helvacioglu, S. Sencan, “Evaluation of intrastromal corneal ring segments for treatment of keratoconus with a mechanical implantation technique”, Indian J. Ophthalmol., 61, 218–225, (2013). C.F. Lovisolo, A. Calossi, A.C. Ottone, “Intrastromal inserts in keratoconus and ecstatic corneal conditions”, In: C.F. Lovisolo, J.F. Fleming, P.M. Pesando, editors. Intrastromal Corneal Ring Segments. A.T. Canelli, Italy: Fabiano Editore, 95–163 (2000). Mediphacos, “Keraring intrastromal corneal ring segments”, http://bit.ly/keraring, accessed, December 11, 2014. E. Coskunseven, G.D. Kymionis, N.S. Tsiklis, et al., “One-year results of intrastromal corneal ring segment implantation (KeraRing) using femtosecond laser in patients with keratoconus”, Am. J. Ophthalmol., 145, 775–779, (2008). doi: 10.1016/j.ajo.2007.12.022. R.B. Küçümen, D. Başar, M.L. Alimgil, “Femtosecond laser assisted intrastromal corneal ring segment (Keraring) implantation in keratoconus”, http://bit.ly/icrs-kc, accessed December 11, 2014.
