
Bac T. Nguyen, glaucoma specialist at the Berkeley Eye Center, based in Houston, Texas, USA: In spring 2021, I joined the Berkeley Eye Center, a large multi-speciality group with 19 ophthalmologists and 31 optometrists, after working as a faculty member at the Baylor College of Medicine for the previous four years. At Berkeley Eye Center, I lead a tertiary glaucoma referral practice where I primarily manage and treat patients with varying types and severities of glaucoma, but I also do see some comprehensive patients. My surgical volume is a blend of cataract surgery, MIGS, traditional glaucoma filtering surgery, glaucoma lasers, and CPC. At Baylor College of Medicine, I also had a tertiary glaucoma referral practice and was the Deputy Chief of Service for Ophthalmology at Ben Taub General Hospital. I was heavily involved in resident and fellow education, and I staffed a vast majority of the MIGS cases for our residents at Ben Taub.
Blake Williamson, ophthalmic surgeon at the Williamson Eye Center, Baton Rouge, Louisiana, USA: I own and operate at a high-volume refractive cataract center. We have seven locations, a surgery centre, and we employ around 190 people, including 15 doctors, and we are a comprehensive practice. I have a “boutique practice” built in to my overall larger practice, where I focus on refractive cataract surgery and LASIK. We have a large glaucoma population in Louisiana, and I decided early on that I wasn’t going to ignore glaucoma in my cataract patients, and – quite suddenly – I started doing a tremendous amount of MIGS surgery. This is how I’ve become known as a “MIGS guy,” even though I’m technically a refractive surgeon.


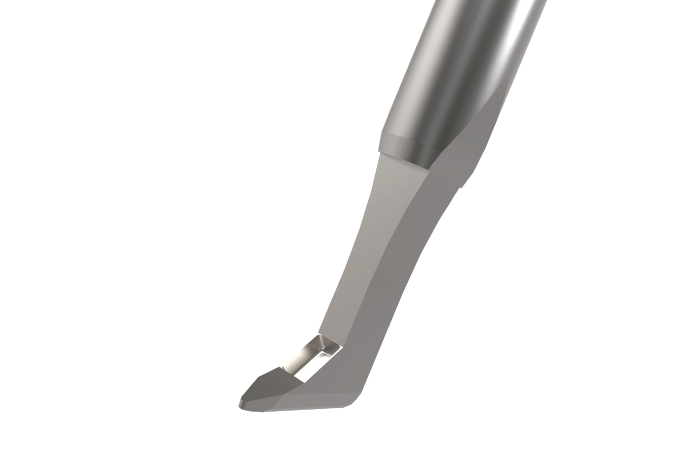
Williamson: The Kahook Dual Blade® was the first MIGS device that I adopted when starting a private practice about five years ago. I’ve been using the new version – the KDB GLIDE® – since the very first week it was commercially available in the US.
Nguyen: I first started using the Kahook Dual Blade® when I was a senior resident, back in 2015, and it has been part of my practice ever since. I first used the new KDB GLIDE® shortly after it was released in 2020 and I have used it since then for my goniotomies. It is my go-to for goniotomy whether I am performing standalone or combination surgery. I have found that the KDB® and KDB GLIDE® provide the most consistent and efficient way to perform a goniotomy.
I have trained residents and fellows on both the original KDB® and the KDB GLIDE®. Goniotomy with the KDB®/KDB GLIDE® is the very first MIGS procedure that I would start my trainees with because of its consistency, efficiency, and favorable safety profile.
Nguyen: Given my tertiary glaucoma referral practice, I see a very wide range of glaucoma types and stages, and perform glaucoma surgery, including MIGS, in a variety of patient types. Goniotomy is unique in ophthalmology – it has been around much longer than a lot of the currently used technology and procedures, and it continues to play an important role in the treatment of glaucoma. Because of its longevity, there is a lot of data in the literature about goniotomy and KDB®. Two particular multicenter studies come to mind which demonstrate the efficacy of the KDB®. Singh and colleagues (1), and Mansouri and colleagues (2) are the studies I like to reference and I find that their results are consistent with the results in my own practice.
Williamson: I’m honored to have been a part of a few different peer reviewed studies with the KDB®, and the results from my clinical practice have absolutely reflected the overall picture. Goniotomy performs really well: patients routinely get the IOP lowered by five to six points, and I can routinely reduce their medication burden by at least one drop with the use of this procedure. That’s been my experience in real-world practice, too.
Williamson: Versatility is the reason why I consider KDB GLIDE® to be such a wonderful tool. It can be used in combination with other MIGS, after other MIGS, in patients with severe glaucoma – the possibilities are endless. I have developed my own algorithm, but it doesn’t mean that the device is not effective in a plethora of different conditions. KDB GLIDE® really shines in my pseudophakic patient population with mild to moderate glaucoma – it’s the tool’s sweet spot for me. If I’m performing cataract surgery in a glaucoma patient, I usually choose stenting, but if they’re already pseudophakic, I go straight for the KDB GLIDE®, especially if the patient has mild or moderate glaucoma. I also like to use it for phakic patients with no cataracts.
Nguyen: The KDB GLIDE® is my most common standalone MIGS procedure. Given its mechanisms of action, this tool is my preferred MIGS solution for patients with angle closure glaucoma, steroid induced glaucoma, pigmentary glaucoma, and pseudo exfoliation glaucoma. As it is not limited to just mild and moderate stage primary open angle glaucoma (POAG) like the trabecular micro-bypass stents are, I am able to perform the procedure featuring the KDB GLIDE® in all stages of POAG. Another unique advantage of the KDB GLIDE® compared to the trabecular micro-bypass stents is that it can be done in standalone on phakic or pseudophakic patients. As with any incisional glaucoma procedure, caution should be taken in patients on anticoagulant and/or antiplatelet therapy.
Nguyen: The three most important advantages I find with the new KDB GLIDE® are: consistency, simplicity, and ease of use.
Williamson: The KDB GLIDE® facilitates a much smoother transition across the canal. With the KDB®, I would sometimes get a little bit of friction from the bottom of the device on the back wall of the canal of Schlemm, and the KDB GLIDE® improvements have solved this issue. The width of the bottom side of the tool has also been reduced to fit more easily within the canal.
Nguyen: As our population ages, and reducing disease burden while improving quality of life become increasingly important, my definition of a successful outcome with MIGS is achieving disease stability with a reduction of glaucoma medication burden. I have found that the KDB GLIDE® provides a consistent way of achieving this by reducing IOP and/or reducing glaucoma medication burden to achieve disease stability with minimal risk compared to traditional glaucoma surgery.
Williamson: I typically use the KDB GLIDE® for pseudophakic patients with uncontrolled mild to moderate glaucoma, so my aim is to either reduce medication burden by one drop or remove the need for adding a drop. If the patient has got higher pressure – above 21 – then it is not uncommon to achieve a drop of seven points with the KDB GLIDE®. If the pressure is lower, starting at 15-18, my main aim is to get the patient the medications, even if the IOP is now lowered by more than a couple of points.
Nguyen: Pre-operative gonioscopy is important when planning any MIGS procedure, and it provides a wealth of important information: (i) You can determine if you need to stain the angle with trypan blue if there is faintly pigmented trabecular meshwork (ii) You can determine if you will need to break up any peripheral anterior synechiae prior to performing your goniotomy (iii) You can determine if the patient has pigmentary glaucoma or pseudo exfoliation glaucoma which – in my experience – tend to respond very well to KDB GLIDE® goniotomy.
Pre-operatively, I ask the patient about anticoagulant/antiplatelet therapy. It is very important as it helps determine if the patient is at risk of post-operative bleeding and hyphema.
Post-operatively, I counsel patients about ways to minimize risk of bleeding, such as keeping their head of bed elevated, avoiding strenuous activity, heavy lifting, or bending at the waist.
In terms of post-operative medication, I tend to keep my patients on steroids longer than my standalone cataract surgery patients, having them use their topical steroid four times a day for two weeks, followed by the normal weekly taper. I also keep my patients on Pilocarpine 2% once a day before bedtime for the first four weeks, as I find that this reduces the risk of PAS formation in the angle postoperatively. They will use a topical antibiotic for one week, and if it is combined with cataract surgery, then also a topical NSAID, just like my routine cataract patients.
Williamson: Many surgeons start with Pilocarpine to reduce synechiae formation post-operatively. Clinicians may also take the patient off blood thinners to reduce bleeding and post-operative edema. I don’t do either of those things as I haven’t found them necessary. If I’m just removing three or four clock hours of TM, it’s very uncommon for my patients to get hyphema that doesn’t clear after a week or two. Overall, I don’t change my pre-or post-operative protocols from my regular cataract surgery protocols.
Nguyen: The most common comparison when we discuss reimbursement in MIGS procedures is how the KDB®/KDB GLIDE® compares to the trabecular micro-bypass stents, and this is where the 65820 CPT code has its advantages.
The trabecular micro-bypass stents can only be done in combination with cataract surgery, not standalone, whereas the KDB GLIDE® with the 65820 CPT code can be done as a standalone procedure.
The trabecular micro-bypass stents are only approved to be done in POAG, mild or moderate stage. The KDB GLIDE® with the 65820 CPT code does not have the same restrictions with diagnosis and staging.
Williamson: It’s one of the easiest procedures to get reimbursement for – almost all insurance providers cover it, including Medicaid, and my experience of billing for it has been overwhelmingly positive. It seems like the goniotomy code has been around forever, having been admitted by Otto Barkan in the 1930s, which makes it very easy to get reimbursed when using the technique.

Williamson: In my experience, the KDB GLIDE® has the shortest learning curve of any MIGS device on the market. If a surgeon is only starting using MIGS, they should really start with the KDB GLIDE® – it’s easy to use, versatile, inexpensive, and easy to bill for. There are so many advantages of it!
Nguyen: The KDB GLIDE® feels very smooth in the surgeon’s hands during the procedure. With the new design, you meet essentially no resistance as you move through the angle and follow the curvature of the globe. The design allows the surgeon to easily visualize and control how large a goniotomy you would like to perform in the nasal angle. It performs consistently despite the wide variety of angles I have encountered.
In terms of ease of use, I find it to be one of the quickest angle procedures to master. Because of this, it is the MIGS procedure I start residents on first, before moving on to trabecular micro-bypass stents.
Williamson: For surgeons who have already done iStent surgery or angle-based surgery, using the KDB GLIDE® should be very intuitive. I would only recommend doing a wet lab with the manufacturer’s representative. For those unfamiliar with the angle, my recommendation is that before you start using the KDB GLIDE®, you use the last couple of cases on your cataract surgery day put viscoelastic in the anterior chamber and on the cornea, get comfortable using the gonioprism, and work on visualising the angle. Using your viscoelastic cannula and pretending that’s the KDB GLIDE®, identify your landmarks in the angle, specifically the trabecular meshwork, working on your angle of approach with the tip of the cannula. I would recommend doing that at least 10 or 15 times before you do use the tool, especially if you’ve never been in the angle before. It’s also very useful to watch surgical videos, many of which are available on YouTube, on my channel and others. I truly think that by doing that, you will be setting yourself up for success.
Nguyen: When I teach MIGS surgery, I always emphasize three points: (i) Visualization (ii) Controlled movements inside the angle and (iii) Minimizing risk.
Angle visualization is the most critical step in any MIGS procedure. Before I allow any resident perform a MIGS procedure, I have them practice tilting the scope and visualizing the angle on routine cataract cases. I then have them practice moving inside the angle using the viscoelastic cannula; that way they are able to get the feel and spatial awareness of movements inside the angle. This allows them to practice controlled movements and develop the dexterity necessary to perform angle procedures. Once those skills are mastered, it becomes much easier to perform any MIGS case. I would then have the residents perform the KDB GLIDE® as their first MIGS procedure, before they start doing trabecular micro-bypass stents because it is a simpler movement inside the angle. In addition, with the KDB GLIDE®, as opposed to the trabecular micro-bypass stents, there is no risk of free-floating hardware inside the eye. After they mastered the KDB GLIDE®, we would then move onto trabecular micro-bypass stents. The reason why the trabecular micro-bypass stents come later in my MIGS curriculum for the residents is because there is a risk of free-floating hardware with the stents, which may have to be retrieved or removed if improperly placed.
In addition, the use of a heavier cohesive viscoelastic such as Healon GV or Healon 5 can help maintain angle visualization, anterior chamber stability, and minimize intraoperative bleeding.
Trypan blue can also help stain the trabecular meshwork, allowing for better visualization for early MIGS surgeons.
Williamson: I feel passionately about this device, as I have been involved in its development, and it’s the first MIGS device that I used regularly after finishing my residency. New World Medical is a great company to work with. I encourage all ophthalmic surgeons to start using the KDB GLIDE®, if they aren’t already. Those who have been on the fence about starting to use MIGS – perhaps reimbursement is a challenge in their country – should definitely try the KDB GLIDE®, as it’s inexpensive compared with other devices, truly versatile, and easy to use.
Nguyen: I am happy to work with anyone at any of the ASCRS Skills Transfer Labs where I typically am on faculty for the MIGS stations!
References
- SK Dorairaj et al., “A multicenter retrospective comparison of goniotomy versus trabecular bypass device implantation in glaucoma patients undergoing cataract extraction,” Clin Ophthalmol, 12, 791 (2018). PMID: 29750011.
- L Salinas et al., “Goniotomy using the Kahook Dual Blade in severe and refractory glaucoma: 6- month outcomes,” J Glaucoma, 27, 849 (2018). PMID: 29979337.
