- Increasing numbers of patients present with concomitant cataract and glaucoma.
- Dealing with both at the same time surgically has been complicated by risks inherent in trabeculectomy and tube shunt placement.
- Medical IOP management with prostaglandins risks inducing or exacerbating inflammation.
- Placing an iStent during cataract surgery reduces IOP, lessening the need for glaucoma medication.
The aging demographic does not just mean an ever-increasing number of patients with age-related eye diseases; it has also generated an explosion in the incidence of co-existing eye diseases. One example of this is the co-occurrence of visually significant cataract and glaucoma. Both are common eye diseases in the elderly, and in some geriatric populations the proportion of patients with both diseases approaches one in five.
The aging demographic does not just mean an ever-increasing number of patients with age-related eye diseases; it has also generated an explosion in the incidence of co-existing eye diseases. One example of this is the co-occurrence of visually significant cataract and glaucoma. Both are common eye diseases in the elderly, and in some geriatric populations the proportion of patients with both diseases approaches one in five. Patients who present with both disorders represent a great opportunity and a big problem. The opportunity is surgical treatment of both conditions in a single surgery – a one-stop shop. This can be a huge bonus for patient and physician alike, saving considerable amounts of time and resources. However, historically, there have been problems. One is that the surgical interventions available to treat glaucoma – trabeculectomy and tube shunts – have risk profiles that confined them to advanced cases of glaucoma. Another is that combining trabeculectomy or tube shunt implantation with cataract surgery is necessarily more complicated, and therefore more challenging to the surgeon to perform, than either procedure alone. Finally, the recovery time is far longer than for cataract surgery alone, so patients undergoing combined surgery need to have expectations of a speedy recovery managed.
Patients who present with both disorders represent a great opportunity and a big problem. The opportunity is surgical treatment of both conditions in a single surgery – a one-stop shop. This can be a huge bonus for patient and physician alike, saving considerable amounts of time and resources. However, historically, there have been problems. One is that the surgical interventions available to treat glaucoma – trabeculectomy and tube shunts – have risk profiles that confined them to advanced cases of glaucoma. Another is that combining trabeculectomy or tube shunt implantation with cataract surgery is necessarily more complicated, and therefore more challenging to the surgeon to perform, than either procedure alone. Finally, the recovery time is far longer than for cataract surgery alone, so patients undergoing combined surgery need to have expectations of a speedy recovery managed.
Medical management
The alternative for patients that present with glaucoma and a cataract that needs to be removed is to continue to medically manage their glaucoma and remove the cataract. This can also be tricky, notably with prostaglandin-based therapies (topical glaucoma medications have minimal risk profiles, even with chronic use). Prostaglandins are part of the inflammatory cascade and can cause ocular inflammation and cystoid macular edema (1,2). They are contraindicated in patients with uveitic glaucoma as they can exacerbate uveitic inflammation, and the same applies post-cataract surgery for at least the first few months in those who are already at an elevated risk of inflammatory complications. This compromises our ability to treat a patient’s glaucoma in the peri- and post-operative period.The burden of medication compliance is also a factor, especially in the postoperative period. Even after a relatively quick recovery from cataract surgery, the self-administration of eye drops multiple times per day, regular checkups with the physician, prescription refills and the possibility of varying side effects is daunting to an elderly patient. For the physician, too, the routine intraocular pressure (IOP) monitoring, additional visual field tests and optical coherence tomography (OCT) imaging and, perhaps most demanding of all, the time spent managing a patient’s medications, add a burden.
It is crucial to ensure that patients understand the importance of adhering to their prescribed regimen, as well as verifying that they are able to instill their drops properly. It is frequently necessary to undergo a “trial and error” process to determine the right drug for each patient. Physicians and their staff are increasingly burdened with managing a patient’s glaucoma therapy while living within the ever-more restrictive formularies of today’s healthcare systems. For the patient, unwanted side effects such as iris color change, darkening around the eyelids, eyelash growth and ocular surface irritation may contribute to a lack of compliance too. Reduction of the medication burden from the patient with glaucoma would be a benefit for both the patient and the treating physician.
The iStent alternative
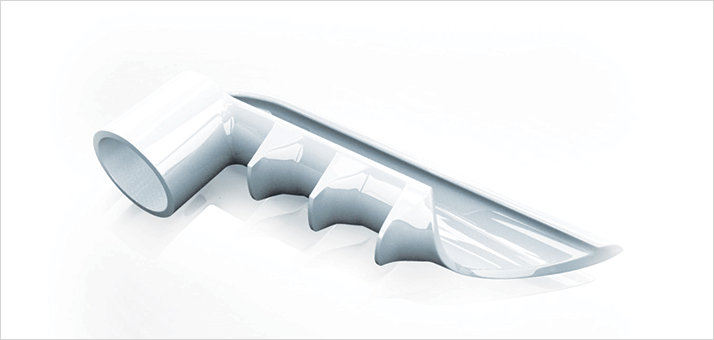
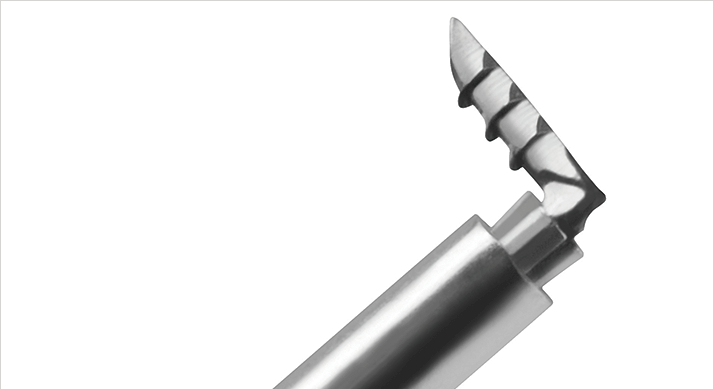
The advent of micro invasive glaucoma surgery (MIGS) has made the management of many cases of coexistent cataract and glaucoma far easier. If possible, I place a micro-bypass stent (iStent, Glaukos Corporation, Laguna Hills, CA, USA) (Figure 1, 2), which is a MIGS device that can be placed during cataract surgery. It can reduce or eliminate the need for glaucoma medications. The device, which is inserted ab interno into Schlemm’s canal using intra-operative gonioscopy, drains aqueous humor from the anterior chamber, through the trabecular meshwork, to the collector channels (Figure 3). It can be placed using a conventional cataract incision and does not require conjunctival or scleral manipulation. The device does not cause bleb formation, dramatically reducing the risk of hypotony and lowering the risk of endophthalmitis compared with the more traditional surgical approaches. In contrast with trabeculectomy or tube shunt placement during cataract surgery, the rate of complications with iStent implantation during cataract surgery is similar to cataract surgery alone, as are the recovery times.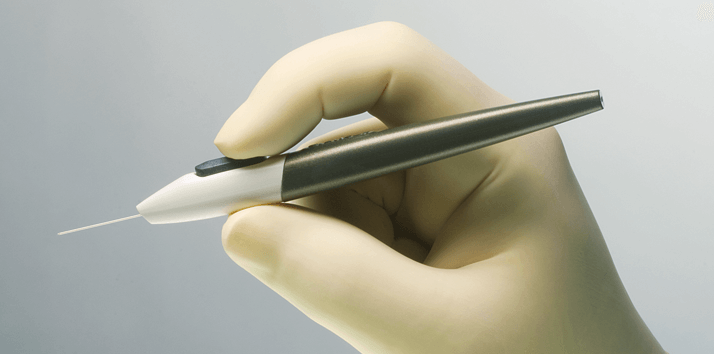
Good recovery times and low complication rates are fine, but there’s no point in implanting such a device if it doesn’t significantly reduce IOP. The American Academy of Ophthalmology (AAO) considers a 20 percent IOP reduction or greater to be “most important” to the patient care process (3). In prospective, randomized, multi-center trials, a single iStent implanted at the same time as cataract surgery resulted in a mean reduction in IOP of 8.4 ± 3.6 mmHg – a greater than 30 percent reduction from pre-implantation levels (4). Two key results arose from this study. First, two-thirds of the patients who received the iStent met the AAO IOP reduction target, whereas only 48 percent of patients who had cataract surgery alone achieved it. Second, 72 percent of patients sustained the target IOPs without the need for topical medication, compared with only half of the control group.
MIGS in general, and drainage devices like the iStent in particular, are an attractive option for many patients with glaucoma that is controlled with medications. If you asked your patients with glaucoma if they would like to have fewer or no medications, I suspect that most would. Devices like the iStent can help achieve this, and they keep all of the alternatives open; if additional treatment for glaucoma or another pathology is required, it can still be performed. For a patient undergoing cataract surgery, the placement of an iStent at the same time minimizes disruption while potentially significantly enhancing quality of life.
The iStent is not a cure for glaucoma, and patients still need to visit their doctor for routine check-ups. The up-side is that these examinations are less intensive, and are required less often. For patients with visually significant cataracts and primary open-angle glaucoma in particular, these benefits are certainly worth considering. Carlos Buznego is a cataract/ refractive surgeon at the Center for Excellence in Eye Care, Miami, FL, USA.
References
- N. Agange, S. Mosaed, “Prostaglandin-induced cystoid macular edema following routine cataract extraction”, J. Ophthalmol., 2010, 690707 (2010). doi: 10.1155/2010/690707. H. Ozdemir, M. Karacorlu, S.A. Karacorlu, “Serous detachment of macula in cystoid macular edema associated with latanoprost”, Eur. J. Ophthalmol, 18, 1014–1016 (2008). American Academy of Ophthalmology Glaucoma Panel, “Preferred Practice Pattern. Primary Open-Angle Glaucoma”, San Francisco, CA: American Academy of Ophthalmology; 2005: 12. Available at: http://one.aao.org/CE/PracticeGuidelines/PPP.aspx. Accessed May 23, 2014. T.W. Samuelson, L.J. Katz, J.M. Wells et al., “Randomized evaluation of the trabecular micro-bypass stent with phacoemulsification in patients with glaucoma and cataract”, Ophthalmology, 118, 459–467 (2011). doi: 10.1016/j.ophtha.2010.07.007.
