The TearLab Osmolarity System offers objective laboratory style data that can help you better distinguish dry eye patients from non-dry eye patients. This diagnostic test guides clinicians in gaining immediate insights into ocular surface health disease, including dry eye disease (DED).
Tear film instability and hyperosmolarity are key signs of DED and can impact visual acuity; 70 percent of total refractive power occurs at the tear film surface (1). Ocular Surface Disease (OSD) can affect the clarity and stability of vision, reduce the accuracy of refractive diagnostic tests, and negatively impact on cataract surgery and LASIK results, leading to refractive surprises and dissatisfied patients. With around 80 percent of cataract patients presenting a sign of OSD (2, 3), it is imperative clinicians have access to objective data to confirm DED or rule it out.
How it works
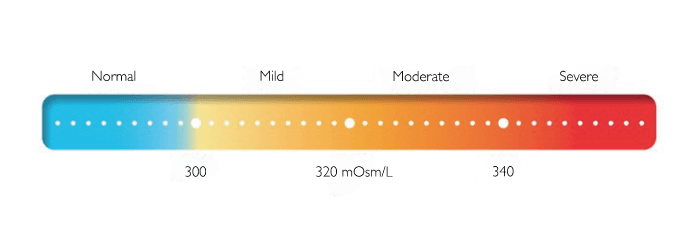
The test requires 50 nl of tear sample – collected at the tear film and transported via microfluidics onto the chip. Osmolarity levels (salt content) is calculated through electrical impedance technology. An osmolarity value is then displayed in mOsm/L and will fall in a range between 290 and 400 mOsm/L (see Figure 1). This value must be interpreted by the clinician, and a diagnosis based on DED severity can be made.
Why test osmolarity?
The TearLab Osmolarity System is the only FDA approved device that measures osmolarity and aids early detection of DED. Elevated (abnormal) osmolarity indicates an unhealthy tear film, which can result in damage to the ocular surface; in fact, elevated osmolarity is the very first biomarker of developing DED (5).
Managing the “Normal” Symptomatic Patient
Osmolarity values, like any laboratory test, has value not only in detecting DED, but also in triggering a further examination if the patient has a normal reading. Put another way, a normal osmolarity reading for a symptomatic patient alerts the clinician that a more detailed investigation needs to be conducted. In 30 percent of cases, symptoms indicative of DED are not caused by dry eye, but by another factor, such as allergies.
Ashley Brissette, Assistant Professor of Ophthalmology at Weill Cornell Medicine, New York Presbyterian Hospital, discusses normal osmolarity – and how useful it is in making a DED diagnosis (5)
In 2018, my colleagues and I conducted a prospective observational cohort study to explore the diagnostic utility of normal tear osmolarity in patients with symptoms suggestive of DED (6). Our aim was to evaluate the presence of any alternate diseases causing DED-like symptoms.
We evaluated 100 patients who reported one or more symptoms indicative of potential DED and subsequently underwent tear osmolarity testing (TearLab Osmolarity System). The patients we included had a normal tear osmolarity test (value <308 mOsm/L in each eye, and an inter-eye difference <8 mOsm/L). The main outcome measure was the presence of any alternative diagnosis to explain the patient’s symptoms.
Among these patients, the mean tear osmolarity was 293.40 mOsms/L (± 6.82), with a mean absolute difference of 2.85 mOsms/L (± 1.98) between the eyes. A possible alternative diagnosis was established in 89 percent of patients with normal tear osmolarity testing. The most frequent diagnoses included anterior blepharitis (26 percent) and allergic conjunctivitis (21 percent). Our study highlights the diagnostic value of a normal osmolarity with an extremely high proportion of patients exhibiting an alternate OSD diagnosis to account for their symptoms.

Clearly, it is important to find out what the true cause is and treat accordingly – and the TearLab Osmolarity System plays an vital role in detecting patients that otherwise could have been treated for DED.
Conclusion
The TearLab Osmolarity test has been used on 20 million eyes in 50 countries over the past decade – and it is predictive of DED 89 percent of the time (4).
The test guides a clinician by providing objective osmolarity values. This data allows a clinician to have a view on the patient’s tear health, even prior to the clinical examination. Finally, the TearLab Osmolarity System is fully reimbursed by Medicare.
References
- 1. D Dawson et al., “Cornea and Sclera,” Duane’s Ophthalmology, Wolters Kluwer: 2013.
- 2. PK Gupta et at., “Prevalence of ocular surface dysfunction in patients presenting for cataract surgery evaluation,” J Cataract Refract Surg, 44, 1090 (2018). PMID: 30078540.
- 3. WB Trattler et al., “The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: the effect of dry eye,” Clin Ophthalmol, 11, 1423 (2017). PMID: 28848324.
- 4. A Tomlinson et al., “Tear film osmolarity: determination of a referent for dry eye diagnosis,” Invest Ophthalmol Vis Sci, 47, 4309 (20116). PMID: 17003420.
- 5. A Brisette, “Putting Dry Eye to the Test,” The Ophthalmologist (2021). Available at: https://bit.ly/3o1s0pO
- 6. A Brissette et al., “The utility of a normal tear osmolarity test in patients presenting with dry eye disease-like symptoms: A prospective analysis”, Contact Lens Ant Eye, 42, 185 (2018). PMID: 30236650.
