Interleukin-18 (IL-18) is a peculiar protein. It is pro-inflammatory, produced by macrophages, and plays a large role in cell-mediated immunity. But researchers at Trinity College, Dublin, Ireland, have demonstrated that rather than damage the retina, IL-18 has the potential to stop choroidal neovascularization (CNV) in its tracks (1). They were led to this surprising discovery by their earlier research that had demonstrated (in mice) that the absence of IL-18 resulted in excessive CNV (2), prompting them to examine whether IL-18 administration could put the brakes on laser-induced CNV progression. The study’s first author, Sarah Doyle said that they “were initially concerned that IL-18 might cause damage to the sensitive cells of the retina, because it is typically linked to inflammation. But surprisingly, we found that low doses had no adverse effects on the retina and yet still suppressed abnormal blood vessel growth.”
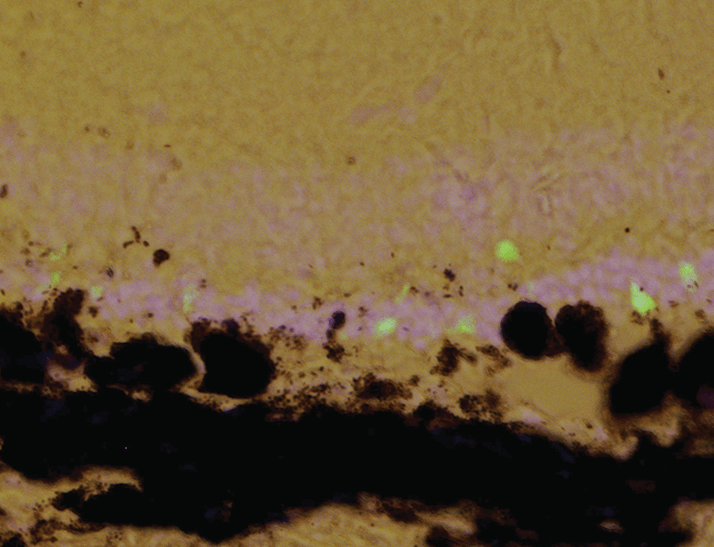
This was promising news, given that the chronic use of anti-VEGF agents risks the development of retinal pigment epithelium (RPE) atrophy. Overexpression of an immature (not fully processed) version of IL-18 – pro-IL-18 – also resulted in the same pathology (Figure 1), but the administration of therapeutic concentrations of IL-18 (the final mature form) did not. Furthermore, IL-18 worked as well as anti-VEGF agents in preventing the swelling that follows laser-induced CNV. Co-administration of both an anti-VEGF agent and IL-18 acted to attenuate CNV development further than either agent alone.
One great potential advantage that IL-18 has is that it can be administered intravitreally or subcutaneously – in mice the drug worked just as effectively by either route. Matthew Campbell said, “GlaxoSmithKline has already started examining subcutaneously-administered IL-18 for the treatment of various types of cancers across some clinical trials, and to date, this method of administration appears to be well tolerated, and IL-18 appears to have a good safety profile.”
If the study results are as applicable to mice as they are to humans, this could mean that ophthalmologists would not necessarily have to administer every IL-18 dose, as is the case with intravitreally-injected anti-VEGF drugs today, helping to lighten their ever-increasing workloads.
Campbell concluded “While it is still early days yet, the fact that IL-18 has already been tested in human subjects and has a good safety profile both systemically and from an ophthalmology perspective, it looks like a promising candidate as we move forward.”
References
- S.L. Doyle et al., “IL-18 Attenuates Experimental Choroidal Neovascularization as a Potential Therapy for Wet Age-Related Macular Degeneration”, Science Translational Medicine, 6, 230ra44 (2014). Epub ahead of print. S.L. Doyle et al., “NLRP3 has a protective role in age-related macular degeneration through the induction of IL-18 by drusen components”, Nat Med., 18, 791-798 (2012). doi: 10.1038/nm.2717.
