
I have been performing corneal collagen cross-linking (CXL) for three years and it has resulted in a paradigm shift in the way we treat keratoconus in our practice, mirroring changes in the standard of care throughout the world. The procedure can have tremendous benefits for patients. According to data from the Dutch National Organ Transplant Registry, the percentage of corneal transplants for keratoconus decreased by approximately 25 percent during the three-year period after CXL was introduced (1).
I now have more than two-year follow-up on patients I have personally treated. What I have consistently observed in these patients is stabilization of their ectatic disease and often corneal flattening, as well. A few treated patients with mild to moderate keratoconus have even been able to achieve 20/25 or better uncorrected visual acuity at the two-year mark, while others are able to successfully correct their vision with glasses or soft contact lenses.
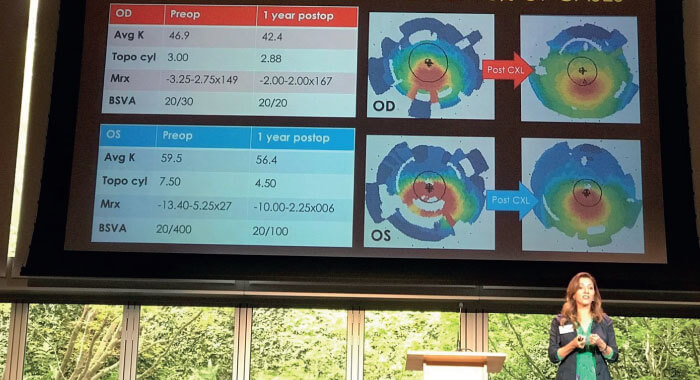
Beyond what this procedure does for patients, I also feel strongly that CXL is a necessary addition to the treatment options offered in any cornea practice treating patients with keratoconus. Offering CXL (see Figure 1) expands my scope of practice and completes the expertise I offer as a corneal specialist to referring doctors and their keratoconic patients.
First, we need to educate our staff about keratoconus, the CXL procedure, and how patients can benefit from it. In my experience, sharing stories about the dramatic impact of this treatment on individual patients has been the most effective way to ensure staff commitment to the new paradigm of treating progressive keratoconus.
Despite the clear-cut advantages of CXL, the patients who would benefit most do not necessarily present on the doorstep of cornea practices. More commonly, they are presenting to primary care optometrists with deteriorating vision and hoping for new glasses or contact lenses. Therefore, it is important to adopt a number of educational strategies to share knowledge with those who are seeing these patients at the first point of contact or offering continuing care to known keratoconics for their specialized contact lenses.
As partners in caring for patients with keratoconus, we need to educate our optometric networks about treatments approved by the FDA, pointers for diagnosis and referral, and what to expect from CXL. My approach has been to communicate with colleagues through clinical e-blasts, social media, one-on-one meetings, presentations at practices that provide specialty contact lenses, educational courses and local optometric meetings (see Figure 2).
Additionally, part of being a good partner is reassuring referring doctors that patients will be sent back to them after CXL as, otherwise, those clinicians will stop referring patients. After all, CXL only stabilizes keratoconus and those patients will still need long-term eye care – and will likely need to be fitted with specialized contact lenses for optimized vision.
From a referral standpoint, the most valuable thing I have done in talking to optometrists is to emphasize the fact that only the FDA-approved procedure is covered by insurance companies, and to reassure them that I will work with their patients to make sure they can have this medically necessary procedure without an excessive out-of-pocket expenditure. We also market outside of the eye-care ecosystem. Just because a practice offers cross-linking doesn’t mean that patients will know that or be able to find the practice when they search online for information about cross-linking or keratoconus. CXL is featured prominently on our website, and we have invested in search engine optimization to increase traffic to our site when people type in relevant search terms.
The goal of CXL is to slow or stop progression of keratoconus, so the earlier we can intervene — before there is significant thinning and vision loss — the better. Progressive keratoconus or ectasia is the indication for CXL, but the definition of progression is not clear cut and is left to the surgeon to determine. It is especially challenging to determine if a patient has progressive disease if they have not had historical objective data on vision or topographic changes.
I try to determine keratoconic progression on the initial consult by establishing if there has been an otherwise unexplained decrease in best spectacle-corrected visual acuity or an increase in manifest cylinder. Corneal topography (evaluating for inferior steepening) is useful in young patients, particularly if you are unsure whether refractive changes are due to keratoconus or simple progression of refractive error. And, of course, advanced topography or tomography can help confirm whether there are early and pathologic changes to the anterior or posterior cornea.
I have asked our optometric network to be on high alert for patients with cylinder changes in the manifest refraction, especially if the eye is not easily correctable to 20/20 without the use of RGP or scleral lenses. Even without corneal topography, this may be enough of a signal that the patient should be referred to a cornea specialist or an ophthalmologist who performs CXL for a formal evaluation.
This would be especially true in younger patients, and ones with risk factors, such as a family history of keratoconus, eye rubbing, or prior LASIK. Insurance carriers have varying definitions for progression, so it is the responsibility of practitioners to learn the requirements of their major carrier(s) for documenting progression. In addition, it is important for a practice incorporating CXL to designate one staff person to keep track of CXL billing and insurance pre-authorizations and appeals.
Patients need to know that, though CXL may slow or stop keratoconus progression, it cannot reverse it. They will need glasses or contact lenses after treatment, but I give them hope that surgical options may be available to correct their refractive error after the cornea has been completely stabilized, such as intracorneal ring segments, implantable contact lenses now available in toric form, topography-guided PRK or a refractive lens exchange.
Patients also need to understand that their vision will worsen before it improves. Research has shown that at the one-month point, K values tend to worsen and steepen, causing visual fluctuations (2). At three months, we start to see a more consistent flattening and are able to prescribe updated vision correction.
We know that keratoconus often presents asymmetrically, so patients will need guidance on the timing of CXL for both eyes. When one eye is diagnosed early, we may be able to perform CXL in just that eye and monitor the fellow eye closely. In more advanced cases, we perform CXL in both eyes, usually two to three months apart, taking care to optimize vision in the first treated eye as much as possible with rigid gas-permeable or scleral lenses before CXL is done on the second eye so patients can function while the eye recovers. Although there are a few marketing, logistical and billing challenges when incorporating CXL into a practice, the opportunity to change the course of a patient’s disease makes it so very worthwhile.
References
- D Godefrooij et al., “Nationwide reduction in the number of corneal transplantations for keratoconus following the implementation of cross-linking”, Acta Ophthalmol, 94, 675-8 (2016). PMID: 27213687
- C Chang and P Hersh, “Corneal collagen cross-linking: A review of 1-year outcomes”, Eye Contact Lens, 40, 345-52 (2014). PMID: 25343263
