You can find almost anything on the Internet these days. But while eBay might be able to provide you with the spare part that you need for your lawnmower, and snopes.com can settle that “is it a hoax?” debate once and for all, things begin to get a bit complicated when it comes to healthcare – eye care included. Peoples’ over-reliance on the Internet as a source of health information is perfectly understandable. Doctor Google doesn’t charge, and will return information aplenty on whatever is asked. Unfortunately, the quality and accuracy of that information can vary considerably, with a plethora of misleading (and sometimes downright inaccurate) advice available, especially when Internet forum posts start to turn up in the search results. We wanted to know what answers patients are looking for. We visited online forums and blogs designed to connect individuals with a progressive ophthalmic disease – keratoconus – to understand exactly what information patients seek, and to establish what their most common questions were. We then posed these questions to a leading keratoconus specialist and researcher, Frederik Raiskup, to compare the expert’s answers with some of the information that patients might find if they look elsewhere.
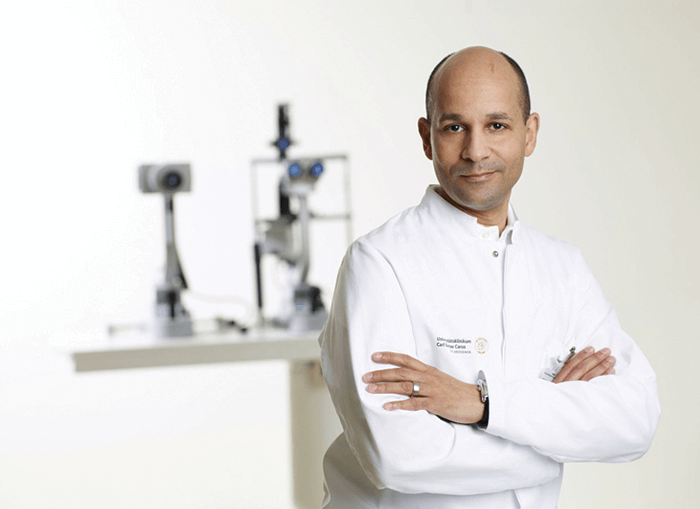
The Expert Frederik Raiskup
- Highly experienced corneal and refractive surgeon and academic researcher
- Medical doctor for over 20 years; qualified ophthalmologist since 1999
- Senior Consultant at the University Eye Center, Carl Gustav Carus Hospital, Dresden
- Graduated PhD in 2008
- A leading authority on keratoconus treatment and a top CXL researcher
(Some) Forum Members
- Have internet-enabled devices and post on forums and Facebook groups
- Mostly well-meaning with helpful intent
- Majority do not have medical training nor access to the biomedical literature
- A small proportion actively disagree with some parts of evidence-based medicine
- Advice is mainly derived from anecdote, rather than evidence
