This non-promotional article is written and sponsored by AbbVie and is intended for ophthalmology healthcare professionals only.
Managing diabetic macular edema (DME), the main cause of vision loss in people living with diabetes, is a complex challenge due to late detection and treatment response variability (1, 2). With deepening understanding of ocular biomarkers and advances in artificial intelligence (AI), healthcare professionals are gaining the tools to swiftly identify DME and deliver timely interventions to help improve patient care (3, 4).
DME is characterized by inflammation, retinal thickening, and macular swelling (2). Some studies suggest that almost one in three people with diabetes are affected by DME (5). When improperly managed or left untreated, progressive retinal damage from DME may severely impair vision (6). “If patients do not respond to treatment, they lose visual acuity,” adds Dr. Mathias Schifflers, International Medical Affairs Head of Eye Care at AbbVie.
How can we use biomarkers to predict how patients will respond to treatment?
Inflammation has a key role in the pathophysiology of DME, driven by several biochemical processes triggered through hyperglycemia (7), says Schifflers. “Unlike other retinal diseases such as neovascular age-related macular degeneration, we see the expression of multiple inflammatory cytokines, broadening possible treatment targets. There are multiple pathways that could be driving the edema; for example, if there is a greater inflammatory component, the edema may be less likely to resolve quickly with anti-vascular endothelial growth factor (VEGF) agents. The presence of various inflammatory cytokines is associated with different DME phenotypes and can be used to help determine prognosis and response to treatment.”
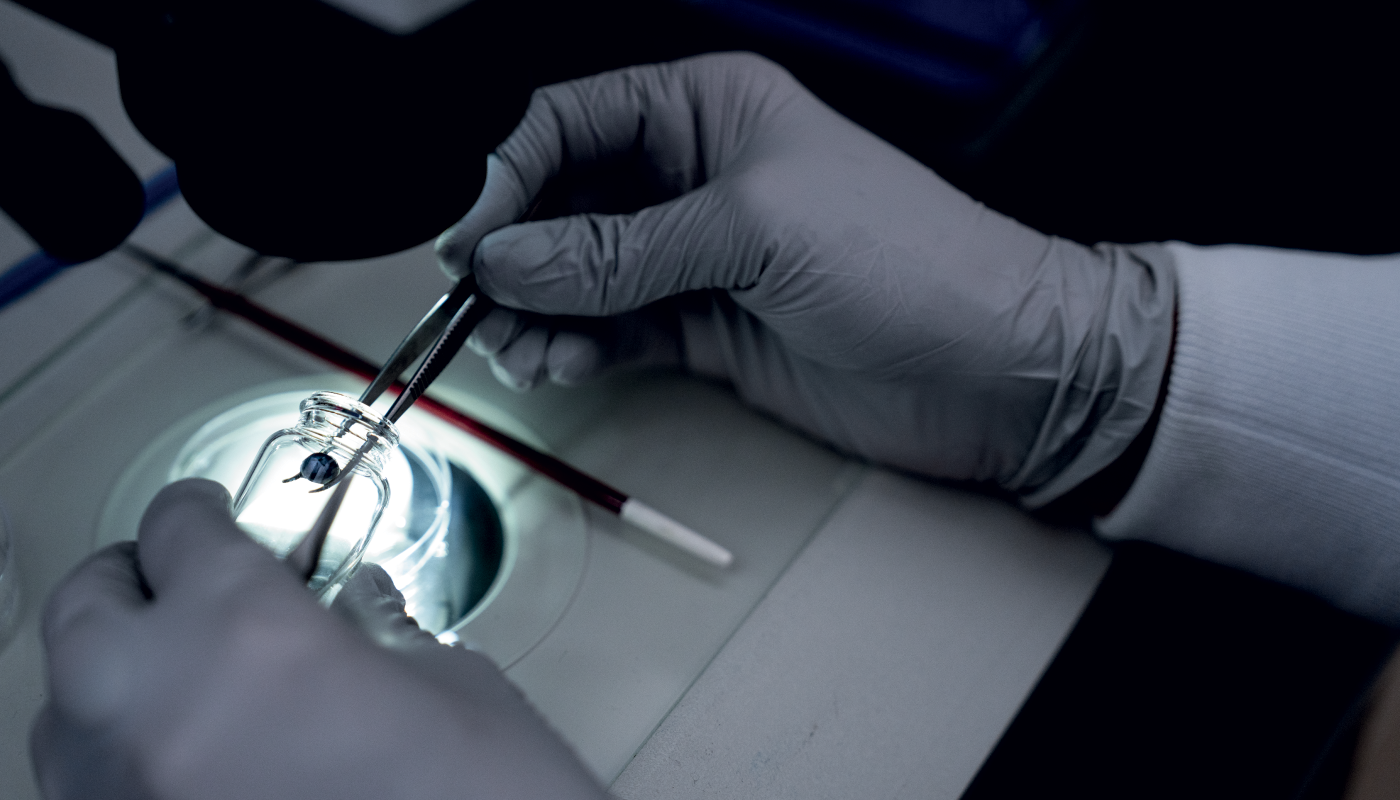
Imaging innovations have changed the landscape of DME through increasingly advanced ocular biomarker detection (8). Dr. Jie Shen, Vice President of Translational Sciences at AbbVie, explains: “Right now, we use optical coherence tomography (OCT) to look at structural features of the disease: at which layer of the retina is the edema? How thick is it – how much fluid has accumulated, especially around the macula?” Shen has decades of experience in ophthalmology and says these retinal thickness measurements can be used to detect severity and location of the edema. Monitoring for changes in these factors is one aspect of measuring DME treatment efficacy (9).
Research shows that certain OCT biomarkers indicate how an eye with DME may respond to different treatment classes, allowing personalized decision-making in patient care (10). “Many groups, including leading retinal experts, have published on the role of OCT biomarkers in predicting response to treatment with intravitreal therapies,” Schifflers observes. “We are conducting studies to understand which patients potentially respond well to specific treatments by analyzing optical biomarkers.” OCT biomarkers such as hyper-reflective foci, outer retinal layer disruption, and intraretinal cysts may help to predict treatment response (10).
How is research and clinical practice evolving now that we better understand the pathophysiology of DME?
“This is where AI comes in,” says Shen. “Even with the most advanced OCT machine, it’s not necessarily at a point that you can delineate exactly which retinal cell layer has edema and readily quantify the edema volume.”
Schifflers adds, “AbbVie is working at the forefront of what science can provide by partnering with AI technology and academic researchers to investigate treatment responses. This will help us to guide treatment using OCT to identify predictive features, really changing the standard of care.”
“AI could predict disease progression based on an individual retina’s structural features, even maybe getting to a point at which it can determine what kind of therapy a person would be most responsive to,” says Shen.
By utilizing technological advances in clinical practice to enable early intervention, healthcare professionals can improve outcomes for people with DME (3).
Schifflers adds: “Some key groups have recognized the value of using biomarkers to tailor treatment to patient phenotype, helping ensure patients are initiated on the treatment most likely to provide an optimal response. As understanding of ocular biomarkers increases and AI devices are validated, treatment decisions will continue to become more personalized, elevating the standard of care.”
ALL-OPHTHDM-240006 | July 2024
References
- S Sharma et al., “Innovations in Diabetic Macular Edema Management: A Comprehensive Review of Automated Quantification and Anti-vascular Endothelial Growth Factor Intervention,” Cureus, 16 (2), e54752 (2024).
- B Bahrami et al., “Diabetic macular oedema: pathophysiology, management challenges and treatment resistance,” Diabetologia, 59 (8), 1594–608 (2016).
- SS Lwin et al., “Utilizing AI to Detect Diabetic Macular Edema in OCT Scans: Performance and Dataset Insights,” IOVS, 65, 2350 (2024).
- L Li et al., “Application of Artificial Intelligence in Precision Medicine for Diabetic Macular Edema,” APJO, 12 (5), 486–94 (2023).
- C Duphare et al., “Diabetic Macular Edema,” in StatPearls [Internet], USA, StatPearls Publishing (2021).
- MA Rose et al., “Adherence of patients with diabetic macular oedema to intravitreal injections: A systematic review,” Clin Exp Ophthalmol, 48 (9), p. 1286–98 (2020).
- EA Urias et al., “Novel therapeutic targets in diabetic macular edema: Beyond VEGF,” Vision Research, 139, 221–7 (2017).
- A Markan et al., “Novel imaging biomarkers in diabetic retinopathy and diabetic macular edema,” Ther Adv Ophthalmol, 12, 2515841420950513 (2020).
- G Trichonas, PK Kaiser, “Optical coherence tomography imaging of macular oedema,” Br J Ophthalmol, 98, no. Suppl 2, p. ii24–ii29 (2014).
- MR Munk et al., “The Role of Intravitreal Corticosteroids in the Treatment of DME: Predictive OCT Biomarkers,” Int J Mol Sci, 23 (14), 7585 (2022).
