Although Optical Coherence Tomography (OCT) scans are widely considered the best diagnostic technique for detecting eye conditions, the images they produce are far from perfect. Due to noise and/or limited axial range, OCT scans are unable to capture all the layers of the retina and choroid – resulting in poor quality images, and thus, poorer quality diagnoses.
New research – from The International Centre for Translational Eye Research (ICTER) in Poland – has managed to find a way around these limitations through the development of Spatio-Temporal Optical Coherence Tomography (STOC-T). This new method makes it possible to view the retina and choroid with high resolution at distinct depths in the frontal section – something that has not been achieved previously.
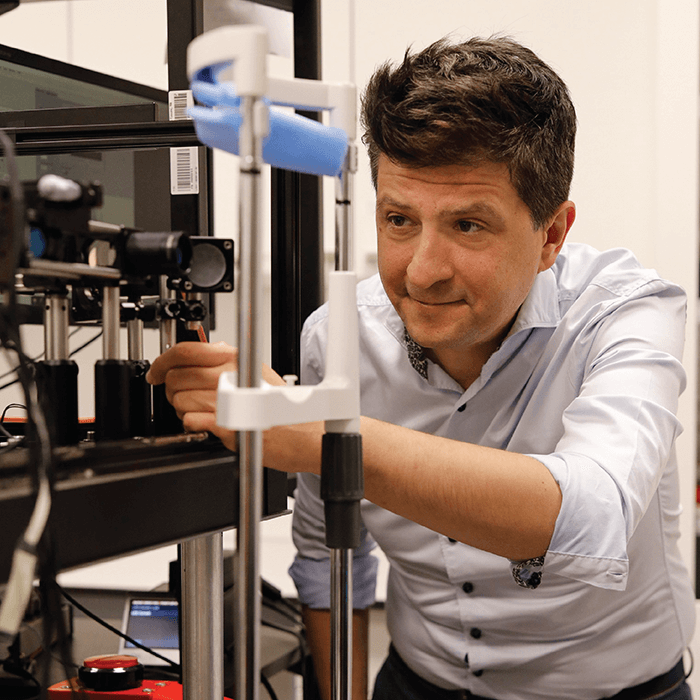
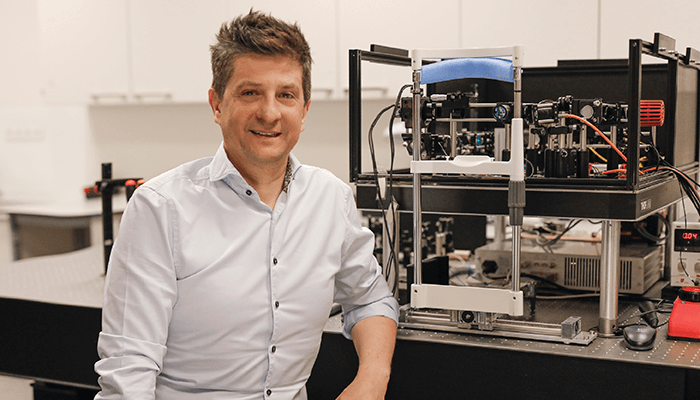
In this article, Maciej Wojtkowski – the lead researcher from the study – speaks about STOC-T’s development, the limitations of OCT, and the future of retinal imaging.
What inspired the development of STOC-T?
The particularity of the OCT method is due to the physical property of the light used: the so-called temporal coherence. Unlike microscopy, this property allows 3-D reconstructions to be obtained. An example of something with a small value of temporal coherence would be lasers with very short pulses or so-called superluminescent diodes. There is another property of the emitted light – spatial coherence. Standard lasers have coherences at a high level, while ordinary light bulbs or LEDs have very low coherences. Although it was known that the quality of OCT images – especially those in coronal projection (en-face retinal images) – are not ideal and deviate from what we see under an ordinary ophthalmoscope, until now, no one has controlled the properties of spatial coherence in OCT. Since the first research on the method and the first SDOCT systems in 1999, I had the idea to take advantage of this property of light. However, it was only recently that we came up with a way to control spatial coherence in a low-cost and simple way. For this reason, we called our technique Spatio-Temporal Optical Coherence Tomography (STOC-T).
Another source of inspiration for this work came from feedback from ophthalmologists who have often pointed out to me that they struggle to visualize the choroidal layers well in OCT images. In fact, other than the ICG fluorescence method, there is no good way to know how lesions are progressing in this extremely sensitive tissue. This is especially true for retinal conditions associated with systemic problems such as diabetes, nephritis, parasites, or uveitis.
The last reason is the increasing need among ophthalmologists to introduce functional methods for retinal examination and replace electroretinography (ERG) with optical methods such as OCT. The STOC-T technique we are introducing guarantees very high phase stability and at the same time accelerates 3-D OCT measurements 50 times over.
What are the limitations of OCT – recognized as it is as the current gold standard of clinical imaging?
Ophthalmologists have been using ophthalmoscopes or fundus cameras for many decades to view the condition of the retina. Much of the intuition in ocular diagnosis is related precisely to images in the plane of the fundus (coronal projection). While available OCT devices are good at reconstructing cross-sectional images, they unfortunately have limited transverse resolution degrading the quality of retinal images in the fundus plane. Even if the spatial resolution were significantly improved, this unfortunately negatively impacts the depth of imaging – that is, we would only see part of the retina (only the layers of pigment epithelium and photoreceptors or only the layers of neurons). To an even greater extent, it is impossible to penetrate the choroid and see its structure with high resolution. In addition, specific noise – also known as speckles – are present in OCT images of the fundus, further impairing high-resolution imaging and the identification of anatomical details or lesions.

How does the new technology work to provide high quality images of the retina and choroid?
To improve the quality of imaging, we use a different method of image reconstruction – called full-field registration – that is not found in classic OCT. Unlike OCT, where the laser beam is focused and scanned onto the retina, here the entire fundus image for different wavelengths is collected. In this way, the images are more like a classic microscope or camera, where defocusing does not result in a loss of recorded light, only a blurring of the image. We are able to compensate for this blurring in the computer using appropriate algorithms. In this way, we obtain fundus images in cross sections of five micrometers and resolution of five micrometers collected from any depth of the retina or choroid.
Despite this, registering full-field OCT with a light source like the one used in traditional OCT would end in complete failure: the highly scattered light in the choroid and pigment epithelium would cover all useful structures and all you would see would be fog. To see the details of the choroid and retinal structures through this fog with high contrast, we need a light source with partial spatial coherence. For this, in turn, we used a long multimode optical fiber that generates hundreds of different patterns of illumination of the sample. Each of these patterns – or modes – exits the fiber with a delay relative to the others. These delays are set by the length and type of optical fiber. The presence of delays for different patterns of fundus illumination allows us to average hundreds of interferometric images on the camera and omit scattering effects and speckle noise.
What are the limitations for the clinical application of this new technology?
Although we have had successful outcomes measuring several patients, after testing the method in the laboratory, the system was found unsuitable for measurement in a clinical setting. In light of this, in the next stages of our research, the system must be converted to a more portable device and adapted to suit clinical working conditions. For high-resolution measurements from the retinal-vascular complex in a standard field of view, a quarter of a terabyte of data must be collected. Although transferring, analyzing, and storing such a large amount of data presents a huge challenge, it is hoped that analyzing the data at the time of collection will significantly reduce the amount of data to be archived.
What does the development of STOC-T mean for the future of retinal imaging and patient care?
We believe that access to images of the choroid will help ophthalmologists better understand the origins of many eye conditions and more quickly respond to early lesions. It may also enable the diagnosis of systemic conditions by providing a more accurate view of the complex vascular system in this part of the eye. We also hope that the quality of imaging can be further improved by the engineering of the device itself. This will enable us to respond to the needs of monitoring and validating new systemic and eye therapies such as pigment epithelial patch implants, gene therapies to restore vision, and precise surgical interventions.