When it comes to vascularized organ transplantation, the donor’s gender matters. Gender mismatches increase the risk of immunological rejection, and the culprit in most cases is H-Y: a male-specific minor histocompatibility antigen (mHA). H-Y epitopes (the part of an antigen that antibodies attach to) derived from intracellular proteins, can be detected by CD4+ T-cells and presented on their surface by the major histocompatibility complex to tell B-cells to make antibodies. This is bad news for the transplanted organ: it’s where immune rejection really kicks in. The bottom line is that there’s potential for male tissue to be rejected when transplanted into females, and this is something that has been observed time and time again in cardiac, pulmonary, hepatic, and (particularly) renal transplantation.
But what about corneal transplantation surgery? A healthy cornea is immune privileged, as it has no blood or lymphatic vessels, sits behind the blood-retina barrier, has few mature antigen presenting cells, and a surfeit of immune-suppressing factors. Patients who undergo keratoplasty receive topical steroid drops during the post-surgical healing period, which penetrate the cornea and act as an immunosuppressant too. Might this mean that the cornea escapes the H-Y mHA-induced misery? Not necessarily. The first (and until recently, the only) signs were present a decade ago, when Böhringer et al. (1) reported that H-Y mismatched – that is, male-to-female (M→F) – corneal transplants were more likely to be immunologically rejected than H-Y matched grafts (i.e. M→M or F→F). Theirs was a small study (229 patients), with a mean follow-up period of two years, and the results weren’t stratified by indication or graft type. But the results were clear: at two years, F→F corneal grafts exhibited an 88 percent rejection-free survival rate; for M→F grafts, the rate was 77 percent. Recently, Hopkinson et al (2) have published the results of a study that examined the influence of gender incompatibility, including H-Y incompatibility, on corneal transplant graft rejection and failure in patients (n=18,171) who had undergone a first corneal transplant (for indications such as keratoconus, Fuchs’ endothelial dystrophy, pseudophakic bullous keratopathy or infection). They fitted a Cox regression model for each indication in order to determine the factors affecting graft failure and rejection at five years, and – after accounting for the effect of other known risk factors – analyzed the impact of gender (including H-Y epitope status) on these outcomes.
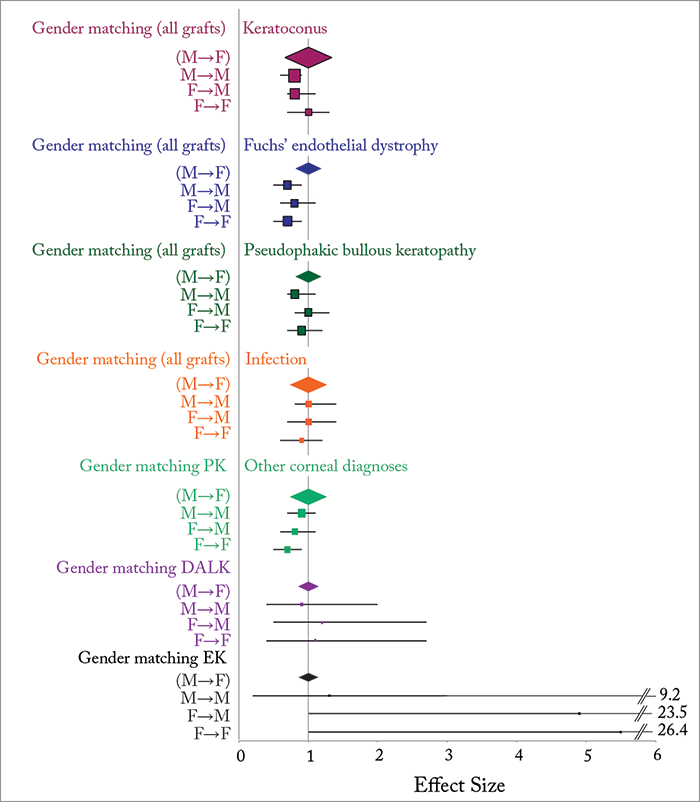
What they found was that H-Y mismatched (M→F) corneas were at greater risk of graft failure or rejection (Figure 1). For patients with Fuchs’ endothelial dystrophy, compared with M→F transplants, F→F grafts were 40 percent less likely to fail (p<0.0001) and 30 percent less likely to reject (p=0.01), M→M were 20 percent less likely to fail (p=0.04) and 30 percent less likely to reject (p=0.01). In patients with keratoconus, M→M matched corneas were 30 percent less likely to fail (p=0.05) and 20 percent less likely to reject (p=0.01) compared with H-Y mismatches. H-Y antigen mismatched (M→F) patients had a greater risk of rejection or graft failure. Stephen Kaye, the study’s corresponding author, called for more research to be performed on this topic: “It is important that other centers in the world investigate these results and undertake similar work. Although it would appear that the effect of gender incompatibility is based on H-Y incompatibility, there may be other gender related factors, which are of importance. We would therefore like to undertake a prospective study, examining in more detail these and other potential factors.”
References
- D Böhringer et al., “Matching of the minor histocompatibility antigen HLA-A1/H-Y may improve prognosis in corneal transplantation”, Transplantation, 82, 1037–1041 (2006). PMID: 17060851. CL Hopkinson, et al., “The influence of donor and recipient gender incompatibility on corneal transplant rejection failure”, Am J Transplant, [Epub ahead of print] (2016). PMID: 27412098.
