Cataract surgery followed by intraocular lens (IOL) implantation is popular with patients – clear vision after years of slow, gradual clouding is a revelation; it improves peoples’ outlook on life, and extends their life expectancy (1).
The procedure is increasing in popularity in almost all developed countries, to the point where it is now the most frequently performed surgery in the world. In the UK, the National Health Service reported a 1.6-fold increase in cataract surgeries between 1998 and 2009 (2); Australia saw a 1.4-fold increase in just five years – between 2000 and 2005 (3), and in one US study in Olmsted County, a 2.5-fold increase was recorded between 1990 and 2010 (4). At one level this isn’t surprising. Developed countries have an increasingly aging population, so the number of procedures performed is expected to increase for purely demographic reasons. However, there is more to the rate increases than that. For example, the Olmsted County data clearly demonstrated that the increase in the number of procedures was greater than that expected for demographic reasons alone (4)
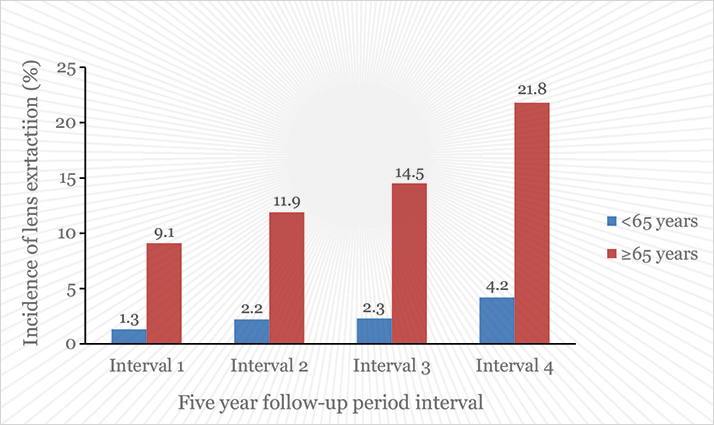
Another series, the Beaver Dam Eye Study (BDES), has shed more light on the issue (5). This longitudinal population-based cohort study recruited people aged 43–84 years during 1987 and 1988, and followed them up every five years. Four follow-ups have now been performed and the resulting analysis published in Ophthalmology (5). The investigators performed ocular exams with lens photography and grading at baseline and at follow-ups, enabling lens opacity to be assessed. They also took medical histories and measurements of blood pressure, height and weight. Adjustments for age and gender were made, as both are known to be risk factors for lens opacities. Analysis of the data revealed that the incidence of lens extraction steepened over the four follow-up periods, from 1.8 percent in the interval between the first and second examination periods, to 11.7 percent in the latest study interval. When split by age (less than 65 years or 65 years and older), it is clear that procedure rates are increasing in both age groups (Figure 1). The increases in procedure rates were associated with better pre-procedural visual acuity at each time point – in essence, surgeons have gradually been reducing the visual opacity threshold before intervening with cataract surgery.
Jay C. Erie’s editorial (6) that accompanied the article couched the developments in terms of “demand and supply”. The past twenty years have witnessed substantial advances in cataract extraction techniques, with ever-improving phacoemulsification methods and iterative improvements of IOLs that leave those from the 1990s as dated as Paisley pattern ties and the Sony Discman. Today, postsurgical complication rates are the lowest they’ve ever been, and refractive outcomes are the best that they have ever been, thanks in part to the introduction of toric IOLs in the late 1990s. The combination of technological advancements mean that cataract/refractive surgeons deliver sharp, long-term vision enhancements to patients that were unimaginable at the start of the BDES study. This may explain the recent spike in the incidence of cataract surgery observed in the youngest age group (55–59 years) in the study; outcomes today are now so good that even patients with incipient cataracts will benefit from surgery. Surgeons can now routinely, reliably and swiftly remove opaque crystalline lenses, and eliminate postoperative spherical or astigmatic errors.
Erie argues that ophthalmologists’ ability to “provide a new, innovative cataract surgery ‘supply’ has provided better outcomes, improved quality of life, and exceeded patient expectations, consequently, and quite naturally this has driven increased patient ‘demand’ for our service,” and notes that the impressive outcomes seen with surgical intervention is driving demand for second-eye surgery – that the initial operation has “changed our patients’ perceptions of disability and visual functioning in the fellow eye.” This much earlier opacity threshold for surgical intervention seems to have arrived without much debate. Surgery is never taken lightly; all interventions carry risk, and it’s the surgeon’s determination of the risk-benefit balance that determines whether the operation proceeds. The risks of adverse events in cataract surgery and IOL implantation are low; combined with better outcomes – particularly refractive ones – patients with incipient cataracts are being cautiously advised to swap their old crystalline lens for an IOL.
References
- C.S. Fong et al., “Correction of Visual Impairment by Cataract Surgery and Improved Survival in Older Persons: The Blue Mountains Eye Study Cohort”, Ophthalmology, 120, 1720–7 (2013).
- HESonline. Main procedures and interventions: 2000-2008. (2009).
- H.R. Taylor, T.V. Hien, J.E. Keefe, “Visual acuity thresholds for cataract surgery and changing Australian population”, Arch Ophthalmol., 124, 1750–3 (2006).
- H.E. Gollogly et al.,“Increasing incidence of cataract surgery: population-based study”, J Cataract Refract Surg., 39, 1383–9 (2013).
- B.E.K. Klein et al., “Changing incidence of lens extraction over twenty years: the Beaver Dam Eye Study”, Ophthalmology, 121, 5–9 (2014).
- J.C. Erie, “Rising cataract surgery rates: demand and supply”, Ophthalmology, 121, 2–4 (2014).
