- Many patients presenting for cataract surgery will have concurrent astigmatism needing correction
- The options are limbal relaxing incisions or toric IOL placement – but which provides the best outcomes?
- I commenced a clinical trial comparing LRIs with a toric IOL in cataract patients in my clinic
- The trial was halted early as it was clear to methat the toric IOL was superior
As a cataract surgeon, it’s essential that you have effective and reliable tools to correct cylindrical error in pseudophakic eyes, as around 15–30% of your patients will have concurrent astigmatism of 1.5 D or more (1,2). My main approach to treating astigmatism up to 2.0 D in patients with cataracts had been to use limbal relaxing incisions (LRI). One study – and in particular, one patient – changed that. Today, I treat patients with cataracts and astigmatism greater than 1.0 D with a toric IOL, reserving LRI only for patients with very mild (<1.0 D) astigmatism.
A change of mind
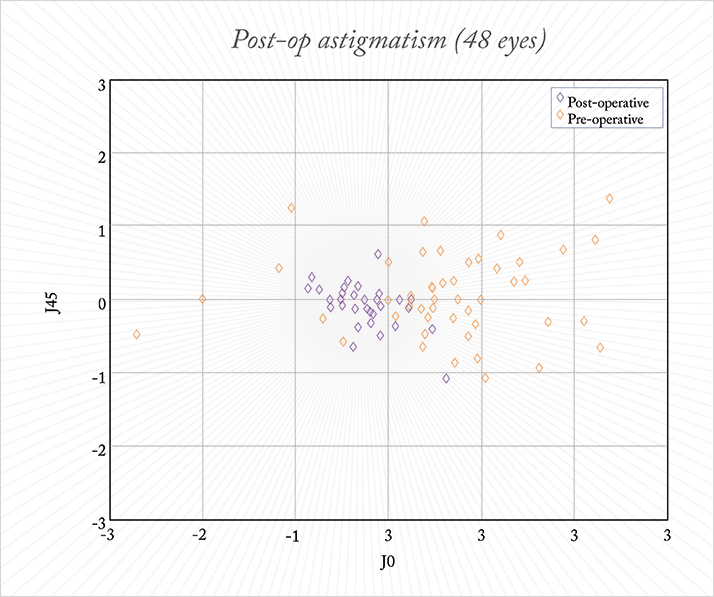
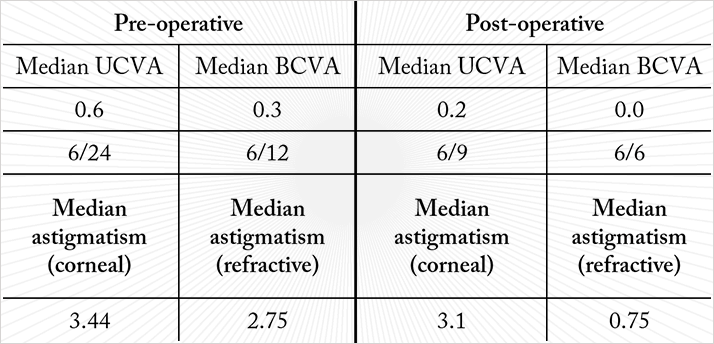
The study I was performing at the time was a comparison of the efficacy of LRI and a toric IOL (T-Flex Aspheric Toric, Rayner Intraocular Lenses Ltd, Hove, UK) for the correction of astigmatism ≥2.5 D in patients undergoing cataract surgery. I had planned to enrol 50 patients into the study and randomize them in a 1:1 ratio to the two treatment groups, but the experience with one patient meant I abandoned the LRI arm after seeing the results from the first 15 patients. The patient who paused the study was a 75-year-old male. He was randomized to receive LRI in one eye and the T-Flex IOL in the other. Corneal astigmatism was comparable in both eyes: 5.1 D in the right eye and 5.5 D in the left. I implanted the T-Flex toric IOL in his right eye and treated the left eye with LRI. His post-operative visual results in the IOL-implanted right eye were good: his unaided vision was 6/9, and his astigmatism was reduced to +0.25 D. The outcomes in the left eye (that underwent LRI) were less impressive. In this case, his unaided vision was 6/18, with 3 D of astigmatism remaining on the refractive plane – understandably the patient was dissatisfied with the vision in his left eye. I resolved this by implanting a Sulcoflex supplementary toric IOL (Rayner Intraocular Lenses Ltd) to correct the residual astigmatism. It was this case that made me totally rethink how I was treating my patients’ astigmatism. LRI risks SIA – surgically induced astigmatism. Every incision changes the cornea, and the larger the incision size, or the closer it is to the center of the cornea, the greater the effect of the astigmatism. LRI often produces variable results, despite the best of efforts. I realized that I should have implanted a toric capsular bag IOL to begin with in this patient, and asked myself if LRI truly was the best option for my cataract patients who had astigmatism of up to 2.0 D? I personally felt it wasn’t. I stopped performing LRI and all remaining patients on this trial received toric IOLs.In the end, the results were good. Among the 48 patients recruited for the T-Flex IOL study, median pre-op vision was 6/24, and there was a wide spread in pre-op corneal astigmatism, with the median at 3.4 D and maximum at 5.5 D. Post-operatively, all patients achieved unaided vision of 6/9 or better and all patients had refractive astigmatism within 1 D (median 0.75 D; Figure 1; Table 1.) However, one patient who received the toric IOL ended up with post-operative astigmatism of 2.75 D. A week after surgery, at the regular follow-up, I took the patient back to the operating room and rotated the lens, after which the patient did very well, reinforcing the importance of correct alignment of toric IOLs.
Starting out with toric IOLs
In treating astigmatic cataract patients, the first and most important step is of course making the diagnosis and determining the correct amount of astigmatism. It is very important to perform keratometry or topography in addition to refraction when diagnosing astigmatism, as the refractive results also include the lenticular astigmatism component. The IOL Master (Zeiss, Jena, Germany) is perhaps the most commonly used test for keratometry, but I prefer to use the Pentacam (Oculus, Wetzlar, Germany). For the best outcomes, I advise patients not to wear contact lenses for 6 weeks if they use hard contact lenses and 2 weeks if they use soft contact lenses before any measurements are made. Once diagnosed, deciding the appropriate power of the IOL to correct the astigmatism is the next crucial step. Most toric IOL manufacturers offer online IOL power calculators. I enter my patient’s data (most importantly axial length, anterior chamber depth, and keratometry readings), and the online calculator performs the power calculations and provides the surgeon with the most appropriate power and axis of orientation. Once the surgeon selects the most suitable IOL, the calculator automatically generates the order directly from the manufacturer.Tips for implanting a toric IOL
Although I find implanting the T-Flex IOL very easy, the best way to familiarize yourself with the lens and this technique is to load the IOL yourself. It is important to remember that this particular IOL has a “reverse S” configuration instead of a “regular S” configuration (Figure 2), meaning that the toric component is on the anterior surface, and the posterior surface still has the square-edge effect to prevent posterior capsule opacity.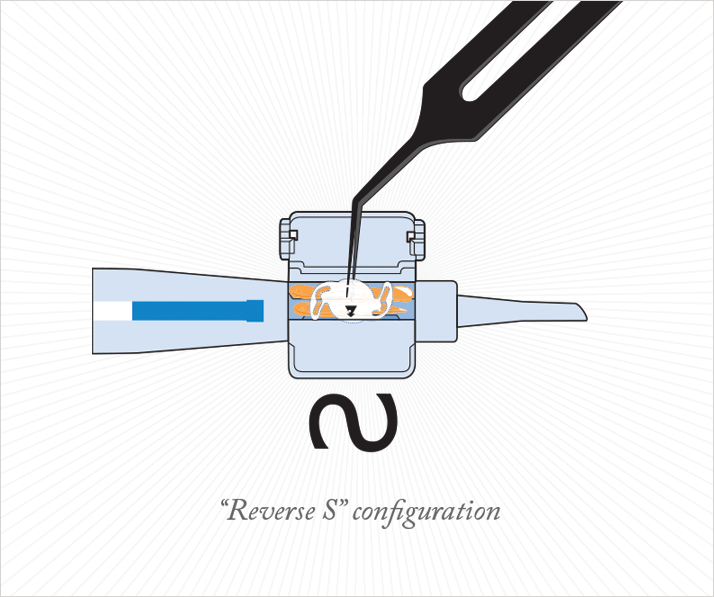
When planning the incision, it is important to remember that the bigger the incision, the greater the surgically-induced astigmatism. I recommend using a 5.0 mm incision and determining what the surgically-induced astigmatism will be. For marking the limbus, the easiest approach is to mark the patient with a slit lamp in the seated position. Once you have a reference point, you can put the Mendez marker at the appropriate axis for the toric IOL.
Alignment is also a very important factor when implanting a toric IOL. If the alignment of the lens is even one degree off, the effect of the IOL can be compromised by 3.3 percent; if the lens is 30 degrees off, the effect of the lens is completely lost (3). In order to get good lens placement, I find it easier to implant the lens about 20 degrees short. This is because the lens tends to rotate and overshoot the target upon removing the viscoelastic. Since it is easier to rotate the lens in the clockwise direction as opposed to in the anti-clockwise direction, I find that implanting the lens a bit short, and then nudging it into the correct position after removing the viscoelastic works best.
Patient selection is important for achieving good results
In general, implanting toric IOLs for the correction of astigmatism is a simple procedure. My results with the T-Flex lens have been excellent right from the start, and have continued to improve over time, and to date, I have managed to successfully correct up to 10 D of astigmatism with this IOL. Of course, as with most cataract and refractive procedures, patient selection is key for achieving high rates of success. Since the T-flex IOL is a capsular bag IOL, it should be avoided in patients with traumatic cataract or previous injury. Toric lenses are also designed for correcting regular astigmatism and should not be used for patients with irregular astigmatism. However, for patients with cataracts and concurrent regular astigmatism, toric IOLs are a fantastic solution. Goodbye LRI.Sanjay Mantry is a Consultant Ophthalmic Surgeon at Gartnavel General Hospital, Glasgow, UK.
References
- T. Ferrer-Blasco, R. Montés-Micó, S.C. Peixoto-de-Matos et al., “Prevalence of corneal astigmatism before cataract surgery”, J. Cataract Refract. Surg., 35, 70–75 (2009). doi: 10.1016/j.jcrs.2008.09.027. M.I. Khan, M. Muhtaseb, “Prevalence of corneal astigmatism in patients having routine cataract surgery at a teaching hospital in the United Kingdom”, J. Cataract Refract. Surg., 37, 1751–1755 (2011). doi: 10.1016/j.jcrs.2011.04.026. C. Novis, “Astigmatism and toric intraocular lenses”, Curr. Opin. Ophthalmol. 11, 47–50 (2000).
