Goniotomy is a safe, simple and effective procedure that promotes enduring IOP reduction by unroofing Schlemm’s Canal (SC). Unlike MIGS stents, which require a targeted approach to allow aqueous outflow, goniotomy exposes multiple clock hours of SC, and several collector channels. Goniotomy also allows surgeons to visualize the white outer wall of SC, confirming completion of the procedure, in a wide range of disease states. Success, of course, depends on physician skill and – crucially – the device used. A common concern with the goniotomy technologies available on the market today is that they may tear tissue, rather than excise it. And that’s understandably problematic, as remaining tissue can cause a blockage of aqueous outflow, which may in turn affect the longevity of IOP reduction. MST considered this carefully when introducing their range of premium Excisional Goniotomy devices. The solution is a trio of technologies designed to excise diseased trabecular meshwork (TM) safely and efficiently: TrabEx, TrabEx+, and Trabectome.
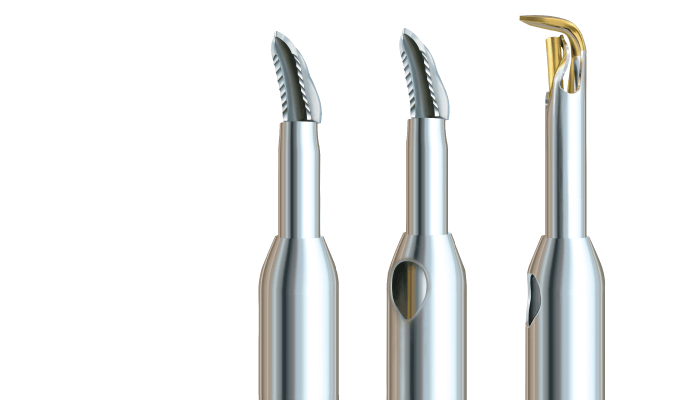
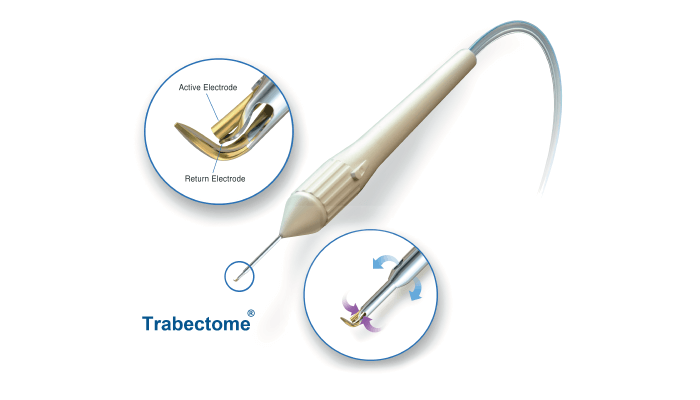
TrabEx features laser-honed serrated blades that promote tissue cutting, while a trapezoidal blade head customizes the excision to varying patient anatomies and promotes optimal TM width removal. TrabEx+ adds Irrigation/Aspiration (I/A), providing maximum visibility by deepening the anterior chamber and allowing better access to the angle (1). I/A also offers the major benefit of managing intraoperative blood reflux by maintaining appropriate pressure in the anterior chamber, preventing blood reflux into the eye (1). Trabectome is the premier option for electrosurgical ablation of diseased TM (2), with a longstanding history of proven clinical outcomes in over 130 peer reviewed articles. The device uses precise electrosurgical ablation to assist complete tissue removal, vaporizing TM without damaging surrounding tissue.
MST’s Excisional Goniotomy product line has been designed to treat the widest possible range of glaucoma conditions, from primary open angle and secondary glaucoma such as pseudoexfoliative or non-pseudoexfoliative glaucoma and more, in both adult and pediatric patients. These devices can also be used with cataract surgery or as standalone procedures.
In a meta-analysis in the British Journal of Ophthalmology, Kevin Kaplowitz and colleagues reviewed 64 studies on Ab Interno Trabeculectomy (AIT) – also known as goniotomy – with the Trabectome and came to the following conclusion: “AIT can be expected to lower the IOP by approximately 36 percent to a final average IOP around 16 mm Hg, while decreasing the number of medications by less than one (3).”
The MST Excisional Goniotomy product line was created with a purpose: to treat everyone, everywhere. To make that possible, the devices are offered at an affordable price and backed by strong reimbursement. All three devices – TrabEx, TrabEx+ and Trabectome – are sold individually. The Trabectome Console is sold separately.
I started using the Trabectome in 2005 when it was still in the clinical trial phase, and began using it in my practice in 2006. I was also fortunate enough to perform the first combined cataract and Trabectome surgery in the world at that time, too. In the years since, I have helped design other instruments in the MST line, including the TrabEx non powered excisional goniotomy blade – and I was the first surgeon to use it clinically. MST Excisional Goniotomy devices have been an important part of my practice for a long time now. It is worth remembering that Trabectome was the first ever angle-based MIGS procedure. Before that, we relied on trabeculectomy, tube shunts, and cyclophotocoagulation. When Trabectome was introduced, it created a whole new
category and I, for one, am grateful.
Goniotomy is the bread and butter of my practice. I use it for open angle glaucoma, anywhere from mild to moderate, as well as more advanced glaucoma cases – either standalone or combined with another procedure that reduces aqueous production to achieve a lower target pressure. We’ve also published data on how the use of goniotomy after tube shunts or trabeculectomy can be effective in patients who have undergone failed glaucoma filtration surgery. I should point out that while goniotomy is suitable for most patients, not everyone is an ideal candidate. I exclude those with significant long-standing angle closure or elevated episcleral venous pressure glaucoma, as well as patients who require a very low target pressure, as this can only really be achieved with trabeculectomy. Aside from these few exceptions, most are eligible for the procedure. The fact that goniotomy can be used as a standalone procedure, suitable for both phakic and pseudophakic patients, adds to its versatility. And it can be performed at the same time as phacoemulsification or cataract surgery, or alongside other minimally invasive or micro incisional surgeries.
The MST Excisional Goniotomy line has delivered a number of benefits to my practice: it has allowed me to offer surgery at an earlier point in the disease, reduce the medication burden on patients, and lower the risk of surgery for patients who don’t necessarily need significant IOP lowering. This latter aspect is useful for individuals who have high pressure, but don’t necessarily need filtration surgery. The other benefit is the design; to achieve optimum IOP lowering, proper removal of the trabecular meshwork is essential – and that means ensuring that tissue is cut, not torn, as tearing leads to bleeding and, in turn, scarring. This quality is what makes MST’s devices so useful; they have been built with precision cutting in mind. In short, tissue cutting, not tearing, is a great advantage. I have also found that the constant irrigation is helpful in maintaining visibility and anterior chamber stability.
References
- C Wang et al., “Angle stability and outflow in excisional ab interno trabeculectomy with active versus passive chamber management”, PLoS One, 12 (2017).
- K Kaplowitz et al., “Techniques and outcomes of minimally invasive trabecular ablation and bypass surgery”, Br J Ophthalmol, 98, 579 (2014). PMID: 24338085.
- K Kaplowitz et al., “ Review and meta-analysis of ab-interno trabeculectomy outcomes”, Br J Ophthalmol, 100, 594 (2016). PMID: 24338085.
