Ophthalmologists rely on – and are trapped by – devices and instruments that run on incompatible software systems. Ophthalmic services would benefit enormously from IT solutions that enable communication between these systems. The development of an integrated IT platform accessible for all – GPs, optometrists, ophthalmologists – could save time, reduce service fragmentation and eliminate sources of error (loss of information, scan mix-ups). For example, improved IT connectivity would assist optometrist-led referrals into secondary care – without the need to go via a GP – which would speed up referrals and relieve GPs of some of the ophthalmology referral burden.
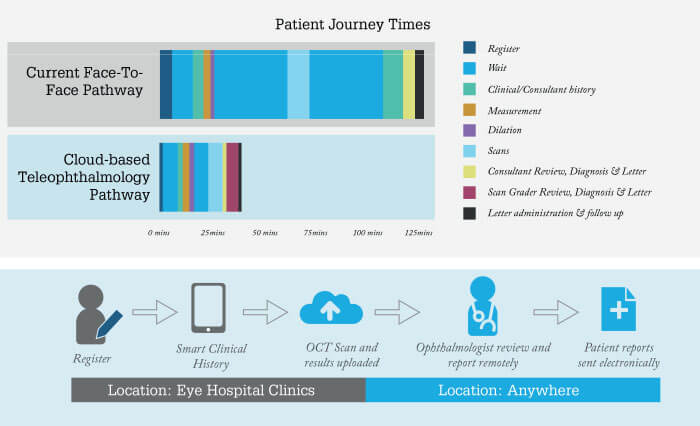
At Moorfields, we are making this vision a reality. Fortunately, we are not alone in understanding the importance of communication technology; the recent NHS “Fit for the Future” plan stipulates a 10-year “digital-first” objective (1). But this revolution will require organizational change; a key requirement is an overhaul of our archaic patient pathways. At present (see Figure 1), these comprise multiple stages separated by periods of waiting. The NHS “digital-first” strategy aims to streamline and compress this pathway via technician-mediated teleophthalmology clinics, followed by location-independent assessment of eye-scan data by graders or ophthalmologists.
But, as noted in the Topol Review – an independent report commissioned by the UK government (2), digital transformation of healthcare systems will depend on appropriate workforce development. Accordingly, the NHS is funding 20 fellowships nationally, across all specialties, in fields relevant to our digital future. Moorfields has won two such fellowships. One involves assessment of Alleye, an approved system that uses a mobile phone app to detect and characterize metamorphosia in patients with retinal conditions.
The object is to reduce hospital visits while improving communication and patient care. The second fellowship aims to assess “Big Picture” – a cloud-based, machine-learning system that uses the “smart clinical history” web app, in combination with Optomed Aurora (a non-mydriatic automated retinal camera). The idea is to perform opportunistic diabetic eye screening at home or in GP surgeries, with asynchronous transfer of retinal images to Moorfields for grading. This initiative hopes to address non-attendance at diabetic eye screening clinics and eliminate the current two-week waiting time for test results.
Moorfields is also expanding its teleophthalmology capabilities in other areas. Our virtual medical retina clinics, introduced in 2016, have been shown to optimize resource use without compromising patient safety or clinical quality (3). Briefly, of 728 patients who were on their second “virtual clinic” appointment were assessed, 497 (70 percent) proceeded to virtual follow-up; 108 (15 percent) were referred to a face-to-face clinic; 107 were discharged; and 17 were referred for urgent treatment. Overall, 542 patients (82 percent) were diagnosed with diabetic retinopathy, and only eight patients were unsuitable for virtual follow-up.
Similarly, an earlier study (4) concluded that Moorfields’ virtual medical retinal clinics improve the efficiency of resource allocation by directing care to those who require treatment, thereby helping medical retinal services meet growing demand. Finally, a retrospective cohort study indicated that a Moorfields cloud-based referral platform – designed to improve communication between optometrists and ophthalmologists – reduces referrals to hospital eye services by over 50 percent (5). Specifically, our system found that 54 of 103 patients who were initially placed into the referral pathway did not need a specialist referral, while 14 were classified as needing urgent treatment. This Moorfields digital-first platform therefore enables rapid-access eye care via referrals from community optometrists, and facilitates essential communication between healthcare providers.
These results confirm our belief that the role of communication technology in eye clinics can only grow. We expect that digital patient portals will increasingly use artificial intelligence-based chatbots to enhance the patient experience and ultimately streamline the patient journey: for example, by reminding patients to take drugs, renew prescriptions, make or keep appointments and manage their self-care. This artificial intelligence assistance may also triage patients by digitally administering questionnaires, and by combining demographic and clinical information with current symptoms. The overall effect will be to speed up processes for both patient and provider.
At the same time, home monitoring will become the norm, we believe; its benefits will include better access for patients to healthcare systems, lower costs and higher efficiency for the NHS as a whole . Similarly, capture of patient-reported outcome measures (PROMS) via the patients’ own mobile devices will allow functional measures to be continually assessed, which will in turn help improve ophthalmic services, support health-related quality of life measurements and cost-effectiveness calculations, and allow those in secondary care to provide timely feedback.
In sum, these developments will push screening and monitoring services into the community, thereby permitting NHS hospitals to focus on treatment of patients. Cloud-based home monitoring, artificial intelligence and workforce evolution – such that ophthalmic nurses, optometrists and technicians operate in extended roles – will allow specialist consultants to attend to those patients who most need their expertise. The end result will be a national health service that provides better care, more efficiently and more conveniently.
This ‘digital-first’ transformation is inevitable, and we at Moorfields are directly involved in its development and implementation, not least in the form of virtual medical retina clinics. Realization of the opportunities that technology provides in the eye healthcare sector will take time – but we are playing a long game in the name of safety, inclusiveness, and quality.
References
- NHS “Fit for the Future” Long Term Plan (2019). Available at: https://bit.ly/2FcJkSe. Accessed July 12, 2019.
- Eric Topol, “The Topol Review: Preparing the healthcare workforce to deliver the digital future. An independent report on behalf of the Secretary of State for Health and Social Care”, Health Education England (2019). Available at: https://bit.ly/2Glxial. Accessed July 12, 2019.
- C Kern et al., “Clinical outcomes of a hospital-based teleophthalmology service: what happens to patients in a virtual clinic?”, Ophthalmol Retina, 3, 422 (2019). PMID: 31044734.
- K Kortuem et al., “Implementation of medical retina virtual clinics in a tertiary eye referral centre”, Br J Ophthalmol, 102, 1391 (2018). PMID: 29306863.
- C Kern et al., “Implementation of a cloud-based referral platform in ophthalmology: making telemedicine services a reality in eye care”, Br J Ophthalmol, [Epub ahead of print]. PMID: 31320383.
