
In the recent past, the gold standard for the surgical lowering of intraocular pressure (IOP) in eyes suffering from glaucoma consisted of performing filtration surgery. These bleb-forming procedures, such as trabeculectomy and tube-shunt implantation, can be associated with significant adverse events, which has led to the emergence of ab interno trabecular meshwork (TM) bypass procedures, including goniotomy (both incisional and excisional), and TM bypass stenting approaches. IOP reduction with ab interno approaches can be achieved by creating an opening between the anterior chamber (AC) and the canal of Schlemm, thereby enabling aqueous humor to bypass the diseased TM to reach the distal aqueous outflow system. But not all TM bypass approaches are equal: incisional goniotomy techniques do not remove TM, leaving tissue leaflets that are prone to closure (1, 2, 3, 4, 5); excisional techniques remove strips of TM, with a more complete treatment that is less likely to fail over time, but which requires well designed tools to achieve full tissue removal, and TM bypass stent implants may fail post-implantation due to fibrotic membrane formation induced secondary to a foreign body reaction (6). How then should surgeons choose between the different bypass options?
Goniotomy techniques
Ammar and colleagues have brought clarity to this issue with a laboratory study of four bypass techniques (7, see Sidebar: Four Goniotomies). Key findings included:
- Suture trabeculotomy incised TM without injury to neighbouring tissue (see Figure 1), but did not excise tissue suggesting a high possibility of closure over time
- Goniotomy with the Microvitreoretinal (MVR) blade (see Figure 2) incised TM, but injured the scleral wall and was associated with significant tissue remnants overlying the canal of Schlemm, suggesting that the opening would be prone to closure over time
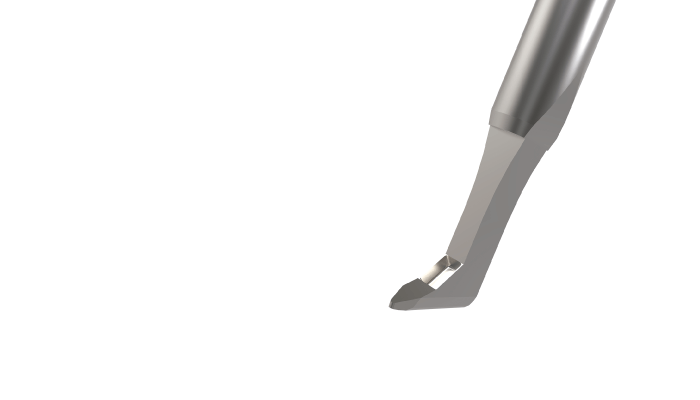
- TrabEx™ (see Figure 3) produced TM excision of variable width, and left large (100-200 micron) tissue leaflets along the entire length of the treated area, suggesting the opening would be prone to closure over time
- Kahook Dual Blade (KDB) GLIDE® (see Figure 4) achieved nearly complete excision of TM without injuring neighbouring tissue; importantly, the procedure left only small (50 microns or less) tissue leaflets in the treated areas, suggesting a lower likelihood of closure over time
Unique features
We might expect KDB GLIDE to outperform non-excisional approaches (such as MVR blade goniotomy or suture trabeculotomy); but why is excisional goniotomy with the KDB GLIDE superior to those of TrabEx, another excisional device? The answer may lie in KDB GLIDE’s design. Its unique non-cutting ramp elevates and stretches diseased TM before parallel incisions are created – here, the benefit is three-fold: it maximizes excision width and minimizes TM leaflet remnants, thus decreasing the risk of closure over time. By contrast, TrabEx has no ramp to elevate/stretch TM; its blades extend to the device tip, such that incision is initiated as soon as the device is inserted in to the TM to reach the canal of Schlemm. This often leads to incision rather than excision of diseased TM. Secondly, KDB GLIDE’s footplate optimizes stability during excision, making for a predictable surgical experience. With TrabEx, excision of a predictable width of TM is difficult to create as it lacks a footplate to stabilize the device against the anterior wall of the canal of Schlemm. Finally, the KDB GLIDE design facilitates device passage within the canal of Schlemm by virtue of smoothly rounded contours and micro engineered dimensions (KDB GLIDE footplate width: 95 microns (8); TrabEx base width: 330 microns; Schlemm’s diameter: ~240 microns (9)).
In summary, when considering these four bypass approaches, only KDB GLIDE offers predictable excision of diseased TM. With more published data than virtually any other non-implant based MIGS device (over 50 papers, level 1 data, four-year follow-up (10)), KDB GLIDE provides surgeons with greater confidence than any other TM bypass approach.
Four Goniotomies
- Purpose: Evaluate tissue-level effects of different goniotomy techniques on human TM
- Design:
- Laboratory investigation using human cadaveric corneal rim tissue (n=4)
- None of the corneal rims had history of past glaucoma surgical procedures or AC surgical procedures other than cataract surgery
- Procedures were completed under microscopic visualization, as follows:
- 360o trabeculotomy (emulates gonioscopy-assisted transluminal trabeculotomy (GATT): 5-0 prolene suture threaded fully around canal of Schlemm, then tightened so as to cut through the entire TM circumference
- MVR blade: used with the intent of cutting into but not through the anterior wall of the canal of Schlemm
-
- TrabEx: positioned in canal of Schlemm and moved forward and then back along an arc, so as to attempt removal of a strip of TM
- KDB GLIDE: the footplate was positioned within the canal of Schlemm, the blade was advanced forward and then back along the same arc so as to remove a strip of TM
- Post-treatment processing: the tissue was fixed in buffered paraformaldehyde, embedded in paraffin, 6 micrometer sections were cut from random locations in treated areas followed by standard H&E staining and microscopic analyses
- Assessment: Sample analysis was completed in masked fashion
References
- L Seibold et al., “Preclinical investigation of ab interno trabeculotomy using a novel dual-blade device,” Am J Ophthalmol, 155, 524 (2013). PMID: 23218696.
- D Grover et al., “Gonioscopy-assisted transluminal trabeculotomy, ab interno trabeculotomy,” Ophthalmol 121, 855 (2014). PMID: 24412282.
- S Gedde et al., “Post-operative complications in the tube versus trabeculectomy (TVT) study during five years of follow-up,” Am J Ophthalmol, 153, 804 (2012). PMID: 22244522.
- S Gedde et al., “Surgical complications in the tube versus trabeculectomy study during the first year of follow-up,” Am J Ophthalmol, 143, 23, (2007). PMID: 17054896.
- Y Amari, T Hamanaka, R Futa, “Pathologic investigation failure of trabeculotomy,” J Glaucoma, 24, 316 (2015). PMID: 23807356.
- C Young et al., “Histopathologic examination of trabecular meshwork changes after trabecular bypass stent implantation,” J Glaucoma, 27, 606 (2018). PMID: 29965891.
- D Ammar, L Seibold, M Kahook, “Preclinical investigation of goniotomy using four different techniques,” Clin Ophthalmol, 14, 3519 (2020). PMID: 33149545.
- Data on file. New World Medical, Inc.
- RDT Hulzen, DH Johnson, “Effect of fixation pressure on juxtacanalicular tissue and Schlemm’s canal,” Invest Ophthalmol Vis Sci, 37, 114 (1996). PMID: 8550315.
- New World Medical Science (2020). Available at: www.nwmscience.com.
