As many as six in every ten patients with glaucoma have ocular surface disease – and this can have a huge impact on their daily lives. We explore why, and what can be done. Many patients with glaucoma have a big problem, and it’s not directly related to their intraocular pressure (IOP): ocular surface disease (OSD), and it can have a huge impact on your patients’ quality of life. OSD is highly prevalent in the general population, and its incidence rises as people age – ranging from 5 to 30 percent in the general population aged 50 years and older (1). As many as 60 percent of patients with glaucoma or ocular hypertension may have OSD – and as many as a third of whom will have the severe form (2). Furthermore, if a patient has glaucoma and OSD, they are up to 12 times more likely to experience symptoms related to their glaucoma medications relative to glaucoma patients without OSD (3).
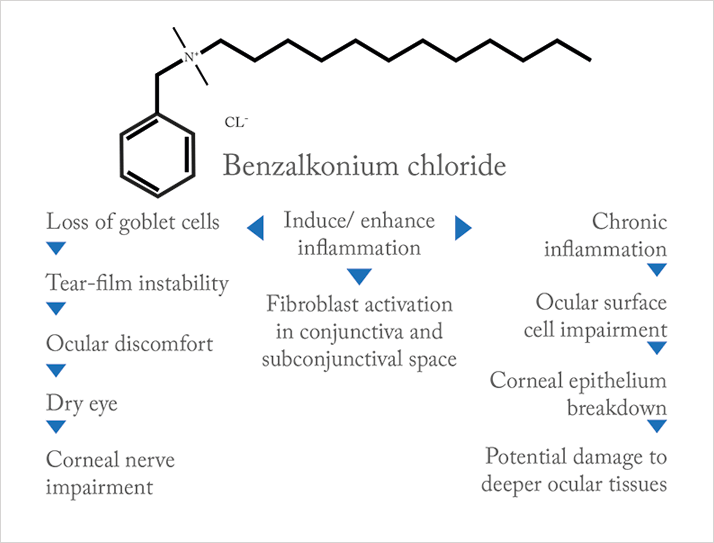
The development of OSD doesn’t appear to be a function of glaucoma per se, rather, it’s related to the type, number and duration of topical glaucoma medications that the patient receives: several studies have shown that there’s a higher prevalence of OSD like dry eye or allergy in patients with glaucoma treated over the long term, and the prevalence rises as the number of topical medications increases. This rise has been linked to preservatives used in the glaucoma medications rather than the active substances (2–6). Given the prevalence of OSD in patients with glaucoma, it makes sense for glaucoma specialists to incorporate a diagnostic routine into their patient assessments. As the time ophthalmologists can spend with a patient in busy glaucoma practices is often brief, the methods used to diagnose and assess OSD need to be quick and simple enough to fit easily in with their daily patient workflow – something like a simple questionnaire completed in the waiting room, and a tear break-up time/ ocular surface staining test should also be considered (5). The elephant in the room is BAC: benzalkonium chloride, a surfactant that’s commonly used in eyedrops as a preservative and bactericide. It dissolves bacterial cell membranes – but it can also have a deleterious effect on the ocular surface, and can be allergenic (Figure 1). As this often results in the patient experiencing OSD symptoms – like itching, irritating or foreign-body sensations – it will have an obvious effect on patients’ regimen compliance, and ultimately, IOP control.
There’s another problem: the number of BAC-containing topical glaucoma medications and the duration of therapy with them can also negatively impact upon the success rates of glaucoma filtration surgery (6,7). As surgical therapy is often necessary to control IOP in a great number of patients who had previously received chronic, topical glaucoma therapy, clearly, BAC is a problem. Fortunately, preservative-free (PF) formulations of a number of topical glaucoma eyedrops are becoming available, and their use could help avoid many of the problems associated with BAC-preserved formulations. So there are ways and means of overcoming the challenges: OSD diagnosis can be performed rapidly and PF medications are now available. There’s undoubtedly a good proportion of patients with glaucoma that also carry the burden of OSD in every glaucoma practice – so screening for these patients and making the appropriate changes to PF-free therapies can not only offer rapid benefits to patients in terms of their OSD, but also means that future filtration surgery is more likely to be successful.
Next month
Should preservative-free formulations of topical glaucoma therapies be the standard of care? The preservatives present in many topical glaucoma medications can result in side effects that have a severely detrimental impact on a significant proportion of patients that receive them – yet the preservatives have no effect on the efficacy of the active drug. As preserved products are associated with an increased rate of side effects, and the presence of side effects are linked to increased glaucoma progression... perhaps it’s time to consider preservative-free formulations to reduce the incidence of these adverse events?
References
- JA Smith et al., “The epidemiology of dry eye disease: report of the Epidemiology Subcommittee of the International Dry Eye WorkShop”, Ocul Surf., 5, 93–107 (2007). EW Leung, FA Medeiros, RN Weinreb, “Prevalence of ocular surface disease in glaucoma patients”, J Glaucoma, 17, 350–355 (2008). PMID: 18703943. C Erb et al., “German register for glaucoma patients with dry eye. I. Basic outcome with respect to dry eye”, Graefes Arch Clin Exp Ophthalmol., 246, 1593–1601 (2008). PMID: 18648841. RD Fechtner et al., “Prevalence of ocular surface complaints in patients with glaucoma using topical intraocular pressure–lowering medications”, Cornea, 29, 618–621 (2010). PMID: 20386433. GC Rossi et al., “Dry eye syndrome-related quality of life in glaucoma patients”, Eur. J. Ophthalmol., 4, 572–579 (2009). PMID: 19551671. DC Broadway et al., “Adverse effects of topical antiglaucoma medication. II. The outcome of filtration surgery”, Arch Ophthalmol., 112, 1446–1454 (1994). PMID: 7980134. C Badouin, “Ocular Surface and External Filtration Surgery: Mutual Relationships”, Glaucoma Surgery. Dev Ophthalmol., [Basel, Karger], 50, 64–78 (2012). JAMA Ophthalmol. 131, 1331–1338 (2013). PMID: 23949096.
