Historically, most surgeons have considered glaucoma to be a contraindication for implantation of a presbyopia-correcting IOL at the time of cataract surgery. For the most part that still holds true, although extended depth of focus (EDOF) IOLs may be considered for patients with mild, well-controlled glaucoma. Additionally, new IOLs in development may mean that we can offer a greater range of vision – even to those with more advanced disease.
Contrast sensitivity concerns
Early in the course of glaucoma, patients begin to lose retinal ganglion cells (RGCs) and retinal nerve fiber layer (RNFL) thickness. These structural changes are associated with functional change, in the form of contrast sensitivity loss, which occurs even before we can measure visual field loss. Contrast sensitivity (CS), while rarely measured in a standardized fashion in glaucoma exams, is likely implicated in a common patient complaint: “It’s getting more difficult to see at night.”
Most presbyopia-correcting IOLs also reduce CS by splitting the amount of light that reaches the retina for distance vision. Healthy individuals may not even notice the reduced contrast, but the combination of a significantly CS-reducing IOL with pre-existing, glaucoma-related CS loss is much more concerning.
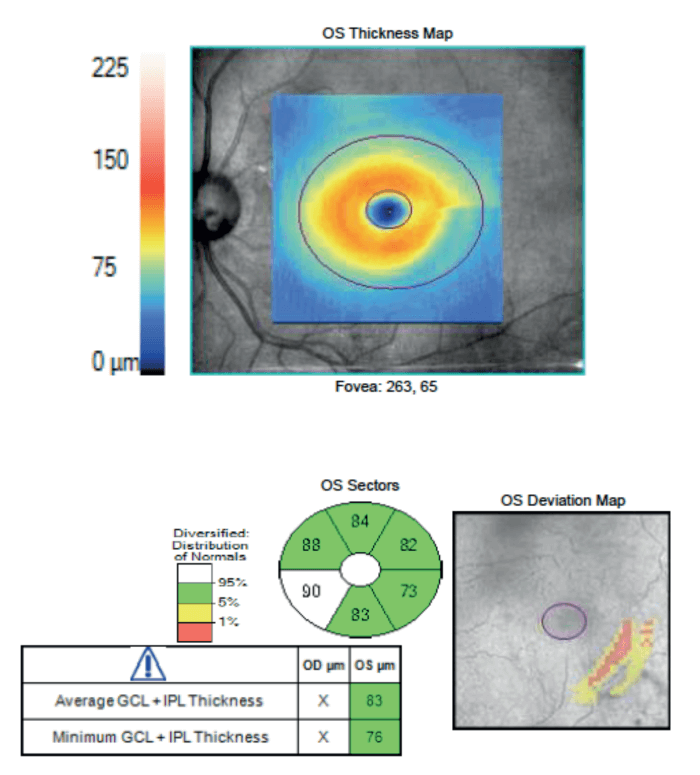
Certainly, not all presbyopia-correcting IOLs are the same. The traditional, high-add multifocal IOLs decrease distance contrast by almost 20 percent. The more recent trifocal lenses (we have several available in Canada, including the Alcon PanOptix lens, the FineVision PhysIOL. and the Zeiss AT-Lisa) decrease distance contrast by about 15 percent. An EDOF lens like the Tecnis Symfony (or in countries where it is available, the Zeiss AT-Lara) reduces distance CS by only about 7 percent. With a 7 percent reduction in CS, I am comfortable implanting EDOF lenses in patients with glaucoma or ocular hypertension who have minimal damage, pressure in the low- to mid-teens and who are well controlled with one or two topical medications (see Figure 1). The product labeling also states that EDOF lenses may be used in patients with early, well-controlled glaucoma.
If these patients desire greater spectacle independence, an EDOF lens is an excellent option – with the caveat that they may require glasses for prolonged near work.
Angle-closure glaucoma
There are only a few situations in which I might consider a trifocal IOL for a glaucoma patient. The most common is in some patients with angle-closure, including primary angle closure suspect (PACS) and primary angle closure (PAC), both situations where there is no structural or functional damage. This form of the disease will be largely addressed by the lens removal itself. In fact, because of the EAGLE study’s findings that lens removal was more cost-effective than laser peripheral iridotomy in primary angle closure glaucoma (PACG) and PAC (1), many surgeons are offering early lens surgery to such patients.
In these cases, the patient may still have some accommodative ability that will be lost with lens surgery, so a presbyopia-correcting IOL may be attractive. There are still some reasons to lean toward an EDOF lens in this population. In angle closure, loose or missing zonules can make the effective lens position (ELP) less predictable, leading to residual refractive error. A highly hyperopic eye with a short axial length is even less likely to achieve emmetropia. Even though these eyes are not likely to see glaucoma progression after IOL surgery, the higher chance of refractive error still makes me more inclined to choose an EDOF lens that is more forgiving of residual error.
We also have to consider the patient’s age when performing early lens surgery for angle closure glaucoma. A 45-year-old angle-closure patient will need that IOL for much longer than their 80-year-old counterpart. In these younger patients, I would prefer a material that is not associated with glistenings, because glistenings tend to worsen in both size and density over time (2).
Unilateral glaucoma
I will also consider mixing and matching a trifocal lens with an EDOF lens in a patient with unilateral glaucoma. I had a patient with mild, well-controlled glaucoma in her left eye, with some RGC damage. In the fellow eye, she had zero damage, good IOP, and seemed not to have the genetic, progressive type of glaucoma. She was very enthusiastic about spectacle independence. I implanted an EDOF lens in the left eye. One week postoperatively, she was very happy with the distance and intermediate vision but (not surprisingly for a myope) liked the idea of better near vision.
I implanted a trifocal lens in her second eye, along with an iStent (Glaukos) for good measure. Although the patient is mostly happy, she has told me that she notices the difference and prefers the quality of her distance vision in the EDOF eye. Since this case, I have been more emphatic that even though trifocal IOLs correct near vision better, the EDOF lens often offers a better quality of distance vision. In cases where we use different IOL technologies in the same patient we’ll often say, “We’re very interested in the difference between the two initially, but in order for your brain to adapt, we don’t want you to keep comparing the two eyes.”
Moderate to advanced glaucoma
What about those patients with more than just mild glaucoma? If they have significant damage, are poorly controlled or on more than two classes of medication already, or have a strong family history of trabeculectomy, we already have proof that their glaucoma (and CS loss) is much more likely to progress. In these patients, I think any presbyopia-correcting IOLs are contraindicated. Even if they have a strong desire for spectacle independence, I will be frank and tell them, “Unfortunately, I think a monofocal IOL is in your best interest long-term.”
In the near future, we may have some new options for patients with moderate to advanced glaucoma. A new generation of EDOF monofocal lenses that offer enhanced intermediate vision is under development. These lenses, which include the Johnson & Johnson Vision Eyhance lens and the Alcon Vivity IOL, do not have any diffractive rings, so they would not be expected to have any detrimental effect on contrast sensitivity or night vision symptoms. These could be a wonderful option for patients who may not be good candidates for EDOF or multifocal IOLs because of glaucoma (or other underlying retinal conditions) but still want to reduce dependence on glasses.
Ocular surface considerations
Finally, no matter which IOL we choose, it is very important to pay attention to the ocular surface and the meibomian glands in patients with glaucoma who desire spectacle independence. Prostaglandin analogs, our first-line therapeutic class for lowering IOP, are closely associated with meibomian gland dystrophy (MGD, 3, see Figure 2). MGD can lead to an unstable tear film, fluctuating vision, and inaccurate biometry and topography, which may lead to improper IOL selection.
Most new biometers, such as the Lenstar and the IOLMaster700, provide an index of measurement quality; alternatively, clinicians can look at the standard deviation between measurements. Glaucoma patients who are going to get a premium lens in our practice have, on average, 2–3 biometry and topography measurements before IOL power calculation is finalized.
Careful evaluation and treatment of ocular surface problems can help ensure that astigmatic correction is accurate and that you meet your patients’ visual goals. While this is true for all patients undergoing lens surgery, it is especially relevant to the glaucoma population with such a high prevalence of MGD.
The author states he is a consultant to Johnson & Johnson Vision, Bausch Health, and Alcon.
References
- A Azuara-Blanco et al., “Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE): A randomized controlled trial”, Trials, 12, 133 (2011). PMID: 21605352.
- A Behndig, E Mönestam, “Quantification of glistenings in intraocular lenses using Scheimpflug photography”, J Cataract Refract Surg, 35, 14 (2009). PMID: 19101419.
- MC Mocan et al., “The association of chronic topical prostaglandin analog use with meibomian gland dysfunction”, J Glaucoma, 25, 770 (2016). PMID: 27513901.
