
I was mentored in my first ophthalmology job in Leicester, UK, by John Sandford-Smith, a much-respected ophthalmologist in the international and low-income setting. I always kept in touch with John, even after he retired, and several years later, he introduced me to William J Williams who’d had an idea for a low-cost ophthalmoscope using LEDs instead of filament bulbs. We chatted and I forwarded on different bits of old equipment he could take apart and play with. Because William likes to keep his head down and out of the “limelight,” John and I have been supporting him over the past few years in developing, evaluating and promoting the device along with several other key people. Contact with the Fred Hollows Foundation, in particular with Richard Le Mesurier, brought seed development money to move to a production version. Through my position in the University of St Andrews Global Health Team, I’ve been well placed to evaluate the device, and present and publish work related to the device. This has led to greater awareness and interest in the Arclight.
International and educational outreach
So far, I’ve supervised a number of different studies evaluating the device in both Malawi and in the UK, and the results so far have been very positive (1)(2)(3)(4). The Arclight is at least as good as traditional devices, and better in some ways. It’s now listed as one of the IAPB’s recommended devices for use in low and middle income settings. One of the major ongoing projects is a large screening exercise of children aged 0–3 years in Uganda and Kenya, which is being driven by the charitable group Sense International. In this, nurses who are on immunization screening programs use the Arclight to screen for media opacities. The program runs until 2019, and will assess the impact of early intervention in infants with vision impairment from cataract and retinoblastoma (5). Similar work is on-going in Tanzania through the International Centre for Eye Health based in London. The Fred Hollows foundation is also currently using the device to screen for trachoma in Ethiopia.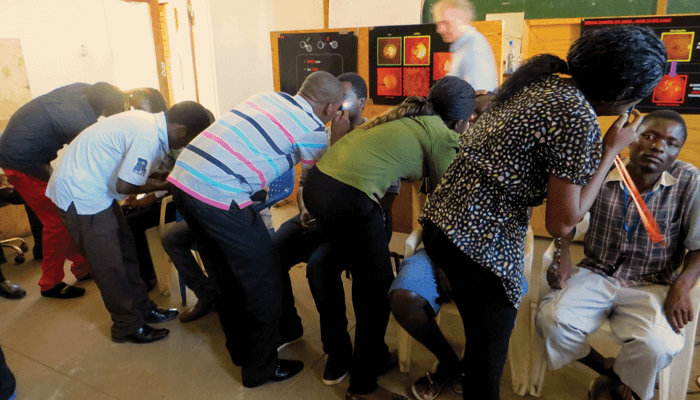
Although improving eyecare in low income and rural settings was the main aim, the device is useful for nearly all physicians. I am a consultant pediatric ophthalmologist and it is my “go-to” ophthalmoscope – I always have one in my pocket in the clinic! I’ve found the magnifying loupe and bright white light extremely useful for examining the anterior segment of babies or small children as you get a very clear view up close. ENT specialists find the device handy in their day-to-day care, and dermatologists like the blue light because it helps highlight certain skin lesions. In the future the aim is to add polarizing filters to the blue light to improve its skin lesion diagnostic capabilities. We have a dermatology colleague trialing a prototype in the field at the moment in Ethiopia. The device is also useful for teaching – it’s an excellent tool to get medical students interested in ophthalmology and fundoscopy (6). Textbooks might feature nice high-resolution, wide-field images of the back of the eye, but in reality ophthalmoscopy is a tricky technique. The field can be small, there are aberrations, and the view can “jump around” and shift in and out of focus. Many medical students have no idea what the back of the eye really looks like through an ophthalmoscope, but attaching the device to a smartphone allows them to see what direct ophthalmoscopy should look like. I’ve been really impressed with the impact of this approach – because students can understand what they are trying to see, they are much more confident at performing ophthalmoscopy. The small size of the device also makes ophthalmoscopy more accessible; physicians carrying the device around their necks or in their pockets might be more likely to perform regular examinations – in turn increasing their confidence and accuracy. It’s important for physicians to be looking at the back of the eye, and if our device can help more doctors do this routinely, I would hope implicitly that this would lead to better healthcare.
The next generation
Right now, as well as being available to low-income countries through the IAPB website, the Arclight is on sale in the UK and Europe via the University of St Andrews online shop. With only seven percent of that revenue going to overheads, 93 percent of the cost goes directly back into distribution, promotion and development of the device in low and middle income countries – Malawi in particular. The School of Medicine in St Andrews and the College of Medicine in Blantyre (Malawi) as well as the eye department in Fife (UK) and the eye department in Lilongwe (Malawi) are twinned, and combined with the historical relationship between Scotland and Malawi, we hope the social business developing around the device will be an important part of the Arclight story. We are also hoping to make the device available to physicians in North America very soon.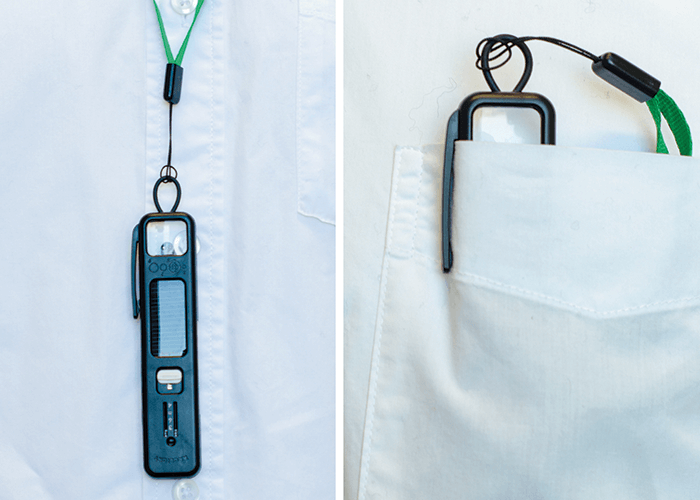
The next iteration of the device should become available later this year, and will feature a programmable switch for greater control over the light settings. It will also include an internal memory chip loaded with teaching and educational material explaining the use of the device, clinical signs to look out for, and suggested treatments and referral pathways for ophthalmic and ENT conditions. We see this as an important tool for rural or field settings as the information can be accessed anytime offline using a micro USB cable and a basic smartphone. Looking further ahead, there are more tools in development that will be also be ultra-low cost, compact and solar powered. There will also be a number of software developments to maximize the diagnostic potential of the devices, and we are actively working with the computer science department here in St Andrews on a few fascinating eye-related projects… It is gratifying to see the impact that the device has had so far. It’s exciting to be involved in the development, evaluation, and promotion of a revolutionary and groundbreaking device. I hope it will continue to have a big impact on blindness and deafness prevention in countries where the access to diagnostic tools is least and the burden greatest. Andrew Blaikie is a Consultant Pediatric Ophthalmologist in NHS Fife, and senior lecturer in the School of Medicine of the University of St Andrews, Scotland, UK.
Making a Difference Globally by John Sandford-Smith Getting the Idea Out There by Andrew Blaikie Bringing the Idea to Life by William J Williams
References
- M Hyrtis, “A cross-over trial comparing skill acquisition between the direct ophthalmoscope and the Arclight ophthalmoscope [Thesis]”. University of Dundee, 2016. S Tuteja, “Comparison of a novel, low-cost, solar-powered pocket ophthalmoscope with a conventional device [Thesis]”. University of St Andrews, 2016. S Blundell, “A mixed-methods evaluation of a novel solar powered low cost ophthalmoscope (Arclight) by healthcare workers in Malawi using the technology acceptance model [Thesis]”. University of Dundee, 2015. J Lowe et al., “The Arclight ophthalmoscope: a reliable low-cost alternative to the standard direct ophthalmoscope”, J Ophthalmol, 743263 (2015). PMID: 26457197. Sense International, “Research study into the effectiveness and impact of early intervention for infants aged 0–3 with complex sensory impairments in Kenya and Uganda”. Available at: bit.ly/SenseScreen. Accessed February 21, 2017. S Tuteja and T Young-Zvandasara, “The Arclight: a ‘pocket’ ophthalmoscope to revitalise undergraduate teaching”, Eye News, 23, (2016). Available at: http://bit.ly/TutejaArclight. Accessed April 04, 2017.
