American and Israeli researchers have developed an implantable sensor that they say measures intraocular pressure (IOP) with high accuracy and reproducibility – when tested in a porcine model (1). IOP is notorious for fluctuating over the course of the day, which makes getting a truly representative measurement with tonometry tricky; posture makes a difference and peak IOP is often not at the time of measurement – it’s when the patient is lying on their back sleeping at night. Furthermore, Goldmann applanation tonometry requires topical anesthesia and can be affected by variations in corneal biomechanical properties, such as thickness or disease state.
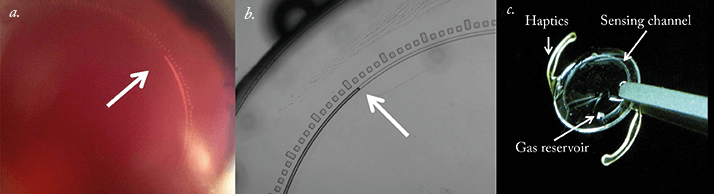
The new device uses a passive pressure sensor implant that relies on microfluidic physics principles. In other words, the implant contains a tiny open channel that draws in the aqueous intraocular fluid (due to capillary forces and IOP), that results in the compression of a gas reservoir attached to the channel. The greater the IOP, the more compressed the gas becomes. To calculate IOP, the relative position of the aqueous-gas interface can be measured with a specialized camera, a slit lap during a routine eye examination – or even a smartphone equipped with an adaptor. The device was originally developed as a stand-alone implant (inserted through the sclera and placed directly against the choroid), but has now been incorporated into an intraocular lens (IOL). IOLs containing the device performed well, first in pressure chamber tests, and also when implanted into the capsular bag of pig eyes as part of a routine cataract surgery procedure. In both cases the relationship between the aqueous-gas interface and IOP was highly linear across the 0 – 16 mmHg pressure range examined. Calibration can be performed in a pressure chamber pre-implantation, and post-implantation via regular Goldmann tonometry. As glaucoma is associated with an elevated risk of cataract development, many patients undergo cataract surgery and receive IOLs. IOLs that also measure IOP sound like an attractive proposition – especially if they enable patients to easily self-monitor using a smartphone.
References
- I.E. Araci, B. Su, S.R. Quake, Y. Mandel, “An Implantable Microfluidic Device for Self- Monitoring of Intraocular Pressure”, Nature Medicine (2014). Epub ahead of print. doi: 10.1038/nm.3621.
