
The rise of anti-VEGF injections has provided new treatment possibilities for countless patients, but also delivered a new challenge: more people need injections than ever before. To tackle skyrocketing demand, we need a way to make injections safer, quicker, and more comfortable for patients. This is exactly what the SP.eye™ from Salar Surgical sets out to do. To find out more about the device, its development, and its advantages, we met with SP.eye inventor and consultant ophthalmologist Sam Evans.
What’s the SP.eye origin story?
When I was training, the anti-VEGF revolution had really just started. In those early days, there were arguments about who was going to get these injections but, even as a junior doctor, the direction of travel was pretty clear – the number of injections was only ever going to increase. When I was an ST3 trainee, I would spend entire days in a small room doing nothing but injections. And that gives you plenty of time to think. It was obvious to me that having only doctors responsible for delivering these injections was never going to be sustainable. What was needed was a foolproof method of delivering these injections – a device that facilitated a simple and, most importantly, safe protocol. A device that would allow anyone to administer injections.
"No one likes intravitreal injections – the speculum is painful and the draping is time-consuming, leading to an experience that is more stressful than it should be."
I also recognized that the delivery method needed to be more comfortable for the patient. No one likes intravitreal injections – the speculum is painful and the draping is time-consuming, leading to an experience that is more stressful than it should be. Now consider that the patient needs to go through the whole process every 6-10 weeks or so…
When I first started injections, they would often take 20 minutes because of draping and checks, so I started sketching out an idea I thought would work. It was basically just a spring on the barrel of a needle. In fact, I think my first prototype was made with the spring from a ballpoint pen, some superglue, and some plastic tubing I had laying around the house. But it worked, so I forged relationships with a medical device consultant and a product designer. Together, we founded a company around the IP, and licensed the design for manufacture. In 2015, the device was granted CE marking and, since then, the device has been distributed around Europe, the UK and Australasia.
And did you hit your safety target?
It’s extremely safe, the needle position is always controlled in three dimensions, and the needle is protected from contamination within the device. Additionally, patients report that they are generally much happier and find the whole process far less stressful than with the traditional technique.
What are the most noteworthy aspects of SP.eye?
I think the first thing that stands out is just how quick it is – I don’t use a speculum, I don’t use a drape. I just ask the patient to look down and then I lift their eyelid up. Next, I line up the caliper on the device with the limbus and inject – it takes about five seconds, if that.
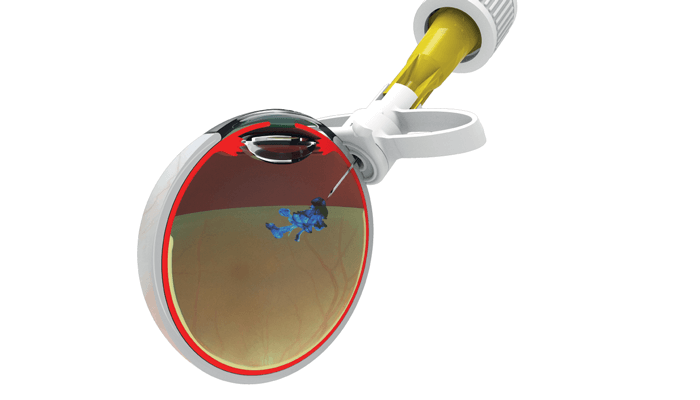
When we were designing the device we wanted to make sure that the needle went to exactly the right place every time and that means controlling the needle position in relation to the limbus; it is always at 4 mm. The device also controls the depth of the injection – dictated by the throw of the spring – which is 6 mm. The angle of the injection avoids the back of the crystalline lens too. All of these design features mean you can do injections one handed because you no longer need to hold a caliper.
Another big safety feature of the design is that it is sharps safe; the needle tip is tucked away and inaccessible; in fact, SP.eye is the only sharps safe intravitreal injection device in the world. An added psychological benefit is that the patient never sees the needle because it is always safely hidden in the barrel of the device before use. Frequently, patients tell us they didn’t feel anything other than a gentle pressure – and that the whole experience was so much easier for them.
Indeed, nearly all patients say they would prefer to have their injections using SP.eye.
What would you say to doctors about introducing SP.eye into their clinic?
Firstly, I would say it will boost efficiency. For private or public hospitals, it is important to treat as many people as possible – as efficiently as possible. Because using this device is so much quicker, I would argue that you could probably see 25–30 percent more patients per clinic. That translates to fewer delays in the whole system, lowered intervals between injections for individuals, and, ultimately, better preservation of visual function for more people.
"She sat on my knee and was curious about what I was doing – I had a needle and a model eye and explained how to give an injection to her."

Secondly, I would say it allows great flexibility within the injection service. Almost anyone can use our device once they’ve been trained; I’ve heard of orthoptists who won’t do injections unless they can use our device. Here’s an interesting short story that further proves the point. When I was developing SP.eye, my daughter was nine years old. She sat on my knee and was curious about what I was doing – I had a needle and a model eye and explained how to give an injection to her. I got her to try an injection with a normal syringe and she stuck it straight through the cornea. Next, I said, “Try SP.eye” and showed her how to line it up. She gave a perfect injection! To say it’s child’s play somewhat trivializes things, but it’s true that it’s a very intuitive device to use.
From the patient perspective, it’s comfortable and stress free. They are often surprised that the injection is so fast and pain free. Patients get very anxious about coming for their injections, and so it’s lovely to use a device which relieves their anxiety - rather than adding to it. I’ve done surveys with my patients, asking them, if they had the choice, how would they get their injections done – with SP.eye or using the traditional route? Around 90–95 percent said they preferred SP.Eye and the others were ambivalent. None preferred the traditional way.
A final big advantage is that SP.eye will allow injections to be given outside the hospital. In other words, we can aspire to take care of people in the community. This mindset is crucial for the future of ophthalmology – not just macula care, but all aspects of the specialty. And though this goal can be challenging right now, my hope is that devices like SP.eye will allow the larger volume of injections to be done outside of the hospital, freeing up resources and helping more people maintain their vision for longer.

