Speaking at the Elios Vision symposium at this year’s Vienna ESCRS, Professor Gus Gazzard, Director of Surgery at Moorfields Eye Hospital and Professor in Ophthalmology, Glaucoma Studies at UCL London, observed that the last few years have seen a huge increase in glaucoma surgical intervention, not least because of the growing understanding that early surgical intervention “can really help our glaucoma patients.” Discussing “phaco plus minimally invasive glaucoma surgery (MIGS),” Prof. Gazzard asserted that “we need phaco-like safety if we are to intervene routinely.” Indeed, not intervening at the time of phaco can present a risk to the patient of a less stable IOP, a faster rate of functional deterioration, reduced ocular surface intergrity/quality and conjunctival health, and a resulting lower quality of life.
The use of an Excimer laser – well-known for its extraordinary precision – to treat glaucoma provides a novel way to lower IOP without the need for implants.
ELIOS is the first Excimer MIGS technology that creates ten “microchannels” (210µm) in the trabecular meshwork using a non-thermal laser. These microchannels facilitate aqueous outflow into Schlemm’s canal, reducing IOP and preserving the integrity and function of the trabecular meshwork. The ELIOS procedure is well suited for combining with Phaco, said Prof. Gazzard, being “elegantly integrated into a normal glaucoma cataract clinic.”
Joining Prof. Gazzard at the symposium was Dr. Paul Ursell of Epsom and St. Helier Hospital UK, who relayed his experiences with Excimer lasers as a cataract surgeon, outlining how the lessons learned from the technology’s 30-year history in refractive surgery will help to support its uptake in glaucoma. Dr Ursell noted that some lasers can have a thermal effect on tissue. However, rather than heating the cells, an Excimer laser ablates at the molecular level, leaving no cellular debris, just plasma.
Prof. Gazzard added that the precision offered by excimer laser for creating full-thickness openings from the anterior chamber through to Schlemm's canal is “particularly exciting” and has “never really been possible before without causing trauma to the trabecular meshwork.” Excimer laser technology allows for a high level of precision. Fig 1 is an X-Ray CT image of human TM. This image shows a very precise ELIOS microchannel perforating the anterior wall of the trabecular meshwork into Schlemm’s canal and illustrates the precision and lack of collateral effect that excimer is known for.
Validating these insights, Prof. Gazzard explained that there is “a substantial amount of data already in the scientific literature” highlighting the 20 publications of ELIOS studies, involving more than 2300 eyes. In an ongoing trial conducted by, Professor Herbert A. Reitsamer, Chairman at the University Eye Clinic, Paracelsus Medical University, demonstrated a drop in IOP of 20 percent in 31 patients three months after ELIOS (Figure 2). “It [IOP] seems to go further down the longer we study these patients,” he added. The Salzburg study concluded that the efficacy of ELIOS is comparable to other minimally invasive procedures used in Schlemm‘s canal, that ELIOS has a good safety profile, and that patients with high pressures at baseline showed higher pressure reductions.
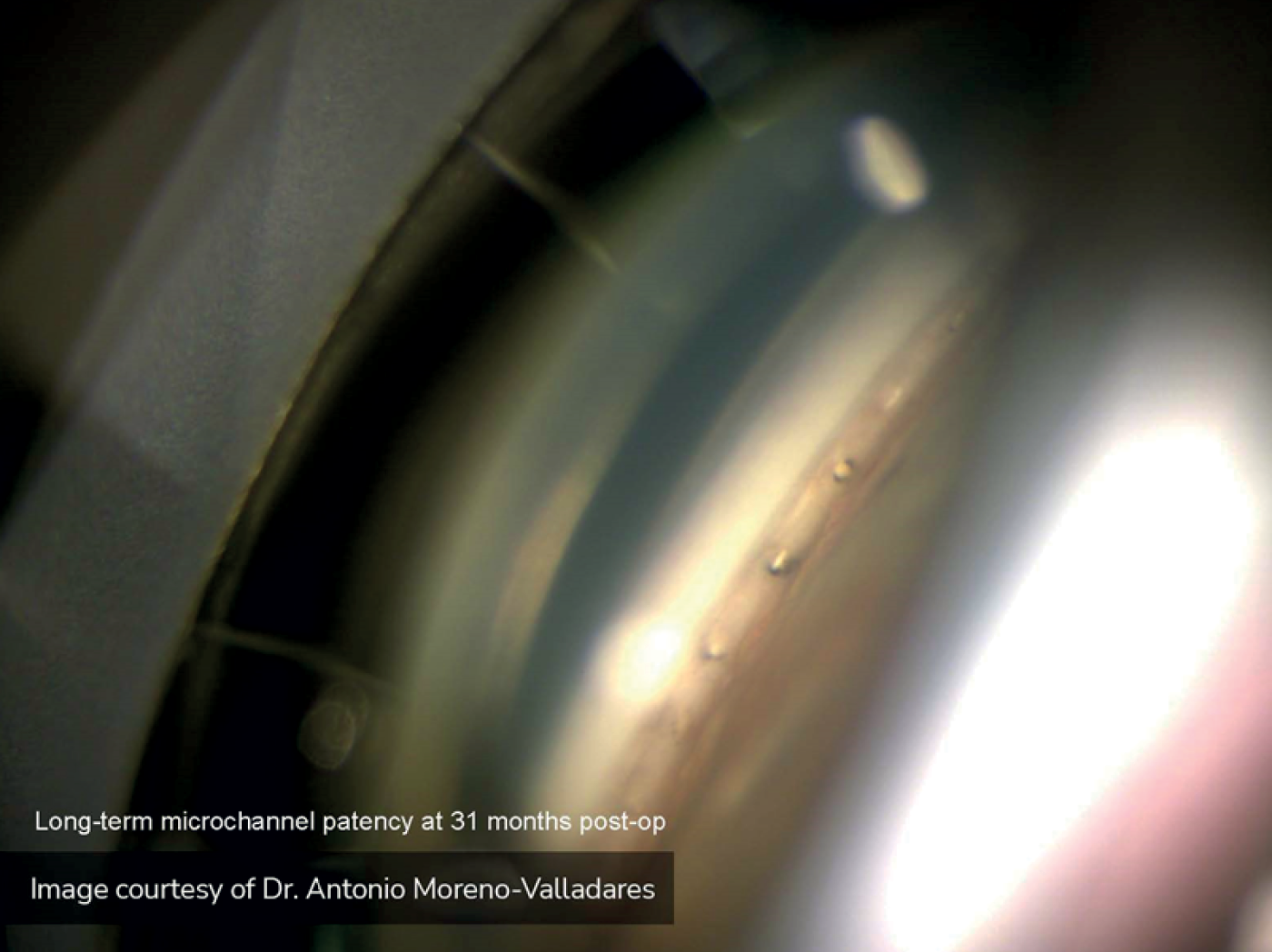
Dr. Antonio Moreno-Valladares of the Hospital Quirónsalud, Albacete, Spain, presented four-year study data on the impact on disease progression, in which he and his colleagues collected data on Phaco-ELIOS procedures performed on 200 patients, mostly with mild open angle glaucoma (1). This study found that, compared with baseline, there was a 35 percent reduction in IOP four years after surgery, with 75 percent of patients medication-free. Dr Moreno-Valladares further commented that, “The retinal nerve fiber layer thickness decrease in ELIOS patients is comparable to physiological age loss”
With ELIOS being used in Europe for over a decade now, even longer-term data has been published (2). Last year, researchers from the University of Zurich published eight-year follow-up results of a study of the ELIOS procedure combined with cataract surgery in 161 eyes of 128 patients (3). The study showed a significant mean IOP reduction from 19.3 mmHg at baseline to 15.4 mmHg after eight years of follow-up (P=0.0040); significant reduction in medication requirements; no observation of serious intra- or postoperative events; and only 3.7 percent of patients requiring secondary incisional glaucoma intervention.
In terms of practical experience of using ELIOS, Dr. Alice Grise-Dulac, ophthalmologist at the Foundation Rothschild Hospital, Paris, spoke about the “learning curve” when adopting the ELIOS procedure. To achieve optimum use of the technology, she outlined the following pearls:
- Vizualisation. Tilt the microscope to between 40-45 degrees and rotate the patient’s head away from you to improve visualization of the angle.
- Preparation and calibration. Work with your operating room team to have the laser calibrated and ready to go by the time you want to perform ELIOS.
- Surgical planning & technique. Plan to treat an area of approximately 3-4 clock hours across the infero- and supero-nasal TM, and ensure your main incision is positioned accordingly. Ensure the probe bevel is correctly oriented ‘up’ and achieves light contact with the TM during microchannel creation. Space each microchannel approximately one probe width apart with the center of the probe in line with the junction between the pigmented and nonpigmented TM.
- Optimize postoperative regimen. Post-operative steroid and antibiotics regimen is the same as with routine phaco, with tapering steroids down over a 4-week period. Personally, I stop IOP lowering medications although some surgeons may prefer to continue medications with some patients, for example, if they are using >2 medications pre-operatively.
“If you follow these steps, your ELIOS learning curve will be short,” concluded Dr. Grise-Dulac.
The application in recent years of Excimer laser technology to the treatment of glaucoma represents the “new frontier of glaucoma therapy,” observed Prof. Gazzard. “We need glaucoma surgery to be as safe, as reproducible, and reliable as cataract surgery,” he noted, adding that he strongly believes that “phaco-plus should be the Gold Standard.”
References
- A Moreno Valladares et al., Arch Soc Esp Oftalmol, March 2021.
- “ELIOS combined with cataract surgery delivers significant IOP reduction out to 8 years,” eliosvision.com, February 16, 2022.
- M Riesen, J Funk et al., “Long-term treatment success and safety of combined phacoemulsification plus excimer laser trabeculostomy: an 8-year follow-up study,” Graefes Arch Clin Exp Ophthalmol. 260, 1611 (2022). PMID: 35034214.
