- There are a number of treatment options for keratoconus, but only corneal cross-linking (CXL) appears to halt the progression of the disease
- To guarantee effective cross-linking, CXL treatment involves removal of the corneal epithelium prior to riboflavin application and ultraviolet light illumination – “epi-off” CXL
- Several methods of “epi-on” (transepithelial) CXL have been proposed, as keeping the corneal epithelium intact should be less painful and help avoid other CXL-associated adverse events
- The evidence so far is that epi-off CXL remains the most effective but transepithelial methods are gaining ground
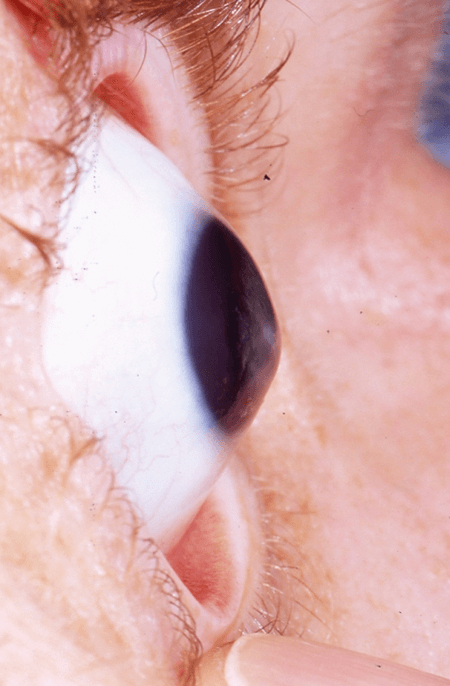
Keratoconus is a common corneal disorder, affecting around 1 in 1,500 of the general population, where the central or paracentral cornea undergoes progressive thinning and steepening to generate the classic cone-shaped cornea (Figure 1). As keratoconus progresses, it results in irregular astigmatism, and scarring begins to occur on the exposed high points of the cornea. This leads to a slow but clear decrease in best-corrected visual acuity (BCVA), with low-contrast visual acuity (VA) deteriorating more rapidly than high-contrast (1,2). It’s not just VA that is progressively lost with keratoconus, though; it’s also quality of life. The disease typically has a young age of onset, and this has two main implications: significantly impaired vision-related quality of life, and the lifetime economic burden of its treatment (3). For context, in 2011, the average annual cost of routine vision care for someone in the US with myopia was estimated to be US$200, whereas the estimated annual price tag for keratoconus was US$653; the lifetime cost of the disease for a single patient, including clinic visits, fitting fees, contact lenses, surgical procedures, and potential complications, was estimated to be US$25,168 (3). It’s a significant, lifelong public health burden. In patients with mild-to-moderate keratoconus, VA is typically corrected with spectacles or contact lenses (and, in some cases, intracorneal ring segment implantation). Advanced disease typically requires corneal surgery, including deep lamellar keratoplasty or penetrating keratoplasty. But if you want an intervention that’s able to slow – and even halt – the progression of keratoconus, you need to look to corneal collagen cross-linking (CXL; Figure 2).

CXL involves a photochemical reaction. Ultraviolet (UV)-A illumination activates riboflavin, which leads to oxidative cross-linking of collagen in the corneal stroma, strengthening the cornea in the process (4) – which is why keratoconus progressions is one of the principal indications for CXL. The procedure is indicated in several circumstances, particularly when keratoconus progression (measured by changes in K values, astigmatism, pachymetry, corneal hysteresis or VA) is evident. Children with keratoconus are at a particularly high risk of progression, which is often rapid, so diagnosis in patients, particularly boys aged under 18 years, is a prompt indication for CXL (5,6).
The history lesson
In clinical use since 1999, the original CXL procedure is known as the ‘Dresden protocol’ (7), and is an “epi-off” procedure (Figure 3). After anesthetizing the eye, the central 8 mm of the corneal epithelium is removed to expose the collagen-rich stroma, and riboflavin solution (0.1% riboflavin-5-phosphate and 20% dextran T-500) is applied to the surface of the cornea both 30 minutes before irradiation and at 5 minute intervals during the course of a 30 minute exposure to 370 nm UVA with a fluence of 3 mW/cm2. After treatment, antibiotic drops are applied and some patients also receive a bandage contact lens. All patients use antibiotics, steroid drops and lubricants postoperatively until re-epithelialization is complete.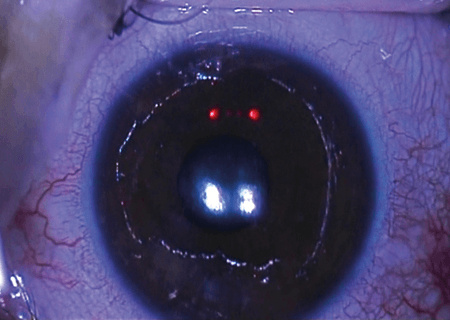
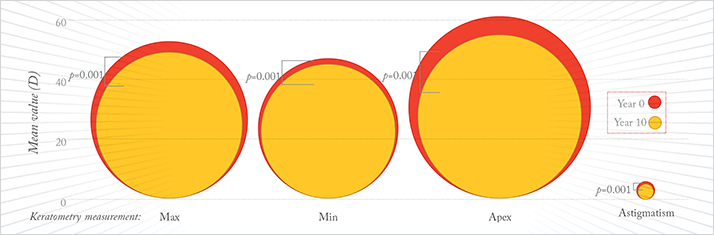
The evidence is that epi-off CXL works – and that its effect lasts for at least 10 years (8), as recently demonstrated by the results of a retrospective interventional case series study
I performed with my colleagues. Our study enrolled 24 patients whose eyes (n=34) were treated with the classic Dresden protocol for progressive keratoconus between the years of 2000 and 2004. Patients’ mean age (standard deviation) at the time of the procedure was 28.4 (±7.3) years, and the mean follow-up period was 10.9 (±1.7) years. We found that on average, compared with baseline values, the maximum keratometry (K), minimum K, and apical K (at the peak of the cone) values were significantly lower 10 years after CXL was first performed – and mean astigmatism was also reduced (Figure 4).
Having said that, a recent systematic review and meta-analysis (9) – which was published before our 10-year study paper (8) was available – did register some concerns, not about the technique per se, but about the quality of the available evidence. Their analysis incorporated 49 studies that involved patients receiving epi-off CXL, of which 39 were graded as “very low quality evidence.” A number of reasons were given, including study design, lack of a comparator arm, high loss to follow-up, and incomplete reporting. The investigators also stated that “uncertainty remains about duration of benefit.” However, they did recognize that “delaying or preventing the need for corneal transplant and improving the fitting of contact lenses could be benefits that are highly valued by people with keratoconus.” Importantly, the most common side effects were pain, corneal edema, and corneal haze, which are usually associated with wound response, but usually resolve within a few days of the procedure. Epi-off CXL also carries a small risk of viral reactivation, haze, melting, infectious ulceration and the development of permanent stromal scars (10). However, most of these adverse events are avoidable or manageable with topical antibiotics, steroids and appropriate peri- and postoperative analgesia. However, it would be nice for patients not to experience these issues.
The transepithelial approach
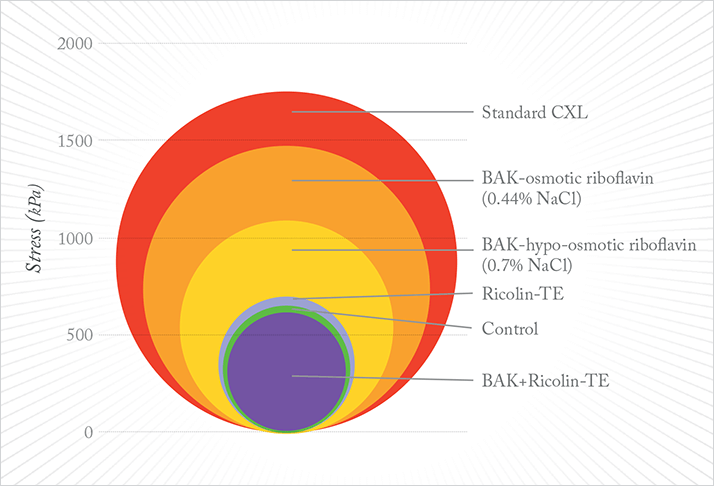
There is another approach: transepithelial (TE) or “epi-on” CXL. Leaving the corneal epithelium intact should eliminate wound-related complications and pain associated with epi-off CXL, the latter being of particular importance in very young patients or those with Down Syndrome (where one in 67 develop keratoconus), and should also lead to a shorter interruption of contact lens wear. Can it work? The reason the Dresden protocol involved epithelial cell removal was the fact that riboflavin is a large hydrophilic molecule that cannot penetrate an intact epithelium; it also doesn’t help that the epithelium blocks about 20 percent of the UV illumination administered. Accordingly, a number of approaches have been taken to try and get the riboflavin to the stroma, including pharmacological cleavage of epithelial tight junctions, intrastromal application of riboflavin through injections or femtosecond laser-created pockets, and iontophoresis.Does it work? A preclinical study (11) performed in rabbits has shown that pharmacological disruption of the epithelial tight junctions with the surfactant benzalkonium chloride (BAK) 0.005% (prior to the regular Dresden illumination and riboflavin application protocol) does increase corneal stiffness – but only by approximately one-fifth of what regular, epi-off CXL achieves. Brillouin microscopy of CXL-treated porcine eyes that had received either an epi-off or TE (with 0.02% BAK and 0.44% NaCl as the penetration enhancers) protocol showed that TE-CXL was 70 percent less effective in terms of biomechanically strengthening the cornea than standard epi-off CXL (12). When evaluated clinically (10), this protocol managed to improve corrected distance VA and corneal topography parameters (including Kmax) on Placido disc topography (EyeSys) remained stable, although the Kmax on Scheimpflug imaging (Oculus Pentacam) and I-S value on Placido topography deteriorated. Treatment failure rates were 7 percent (similar to epi-off CXL failure rates in the literature), and no haze or other complications were noted in the 18-month follow-up period reported. Another study that used different penetration enhancers both for a 30-minute pretreatment soak and throughout the 30 minute illumination period (riboflavin 0.1%, dextran T500, trometamol and EDTA; Ricrolin TE) appeared to halt keratoconus progression with a statistically significant improvement in VA and topographic parameters – according to Placido topography (Optikon Keratron Scout 2000). Another study, using Ricrolin TE for TE-CXL resulted in keratoconus instability, particularly in patients aged 18 years and younger. The study reported that “50 percent of pediatric patients were retreated with epi-off CXL due to significant deterioration of all parameters after 12 months of follow-up” (13). A number of riboflavin solutions have now been, and their transepithelial corneal stiffening effect has been compared relative to standard epi-off CXL in rabbits (Figure 5), with epi-off CXL having the greatest effect (14).
A summary of recent clinical studies of epi-on CXL is presented in Table 1, but please let me draw your attention to the last one in the list (15): the protocol involved instilling gentamicin, BAK and EDTA for three hours, followed by oxybuprocaine for 30 minutes. Riboflavin 0.1% in 20% dextran T500 and oxybuprocaine were then instilled for 30 minutes, finally being followed by 30 minutes of UV-A irradiation to the central 7.5 mm of the cornea while riboflavin was instilled every 5 minutes. I would argue that there would be few epithelial cells left after that process and question its nomenclature as an “epi-on” procedure.
Femtosecond laser pockets
What about using a femtosecond laser to create a localized corneal pocket for riboflavin infusion? Pig eye studies have shown that “the biomechanical effect of CXL using the femtosecond laser pocket technique is about 50 percent less pronounced than that after standard CXL” (16), and it has been tried in the clinic too. John Kanellopoulos performed a small trial, taking ten eyes with early keratoconus, using the femtosecond laser to make an incision 100 µm in depth, and irradiating the eyes with UV-A illumination with a fluence of 7 mw/cm2 for 15 minutes (17). Initial outcomes were good in terms of mean uncorrected and best spectacle-corrected VA, and no ectasia progression (as determined by keratometry) was noted during the mean 26 month follow-up period. It shows promise, but the data aren’t there yet.Iontophoresis
Another method under active investigation is the iontophoretic delivery of riboflavin into the corneal stroma (Figure 6). Riboflavin is water-soluble, negatively charged at physiological pH, and has a low molecular weight – all of which means that the application of a low-intensity electrical current flowing between a negatively charged delivery electrode placed on the cornea and a counter electrode (placed on the patient’s forehead) should be able to drive riboflavin across the intact epithelium and into the corneal stroma.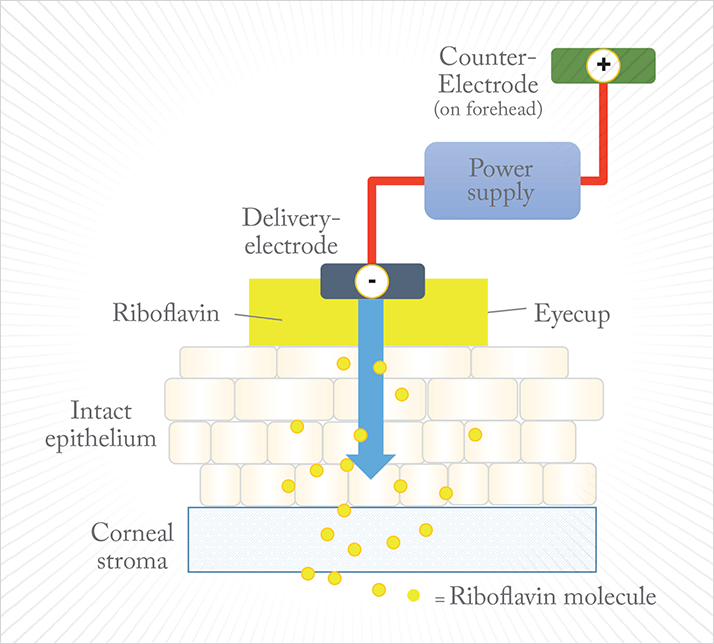
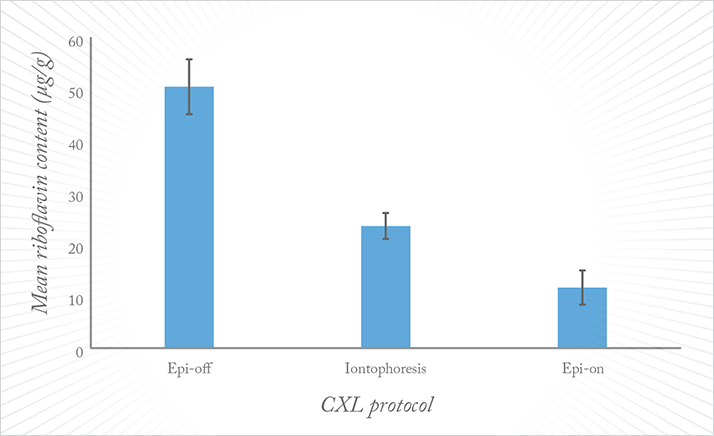
As it turns out, the composition of the solution in which the riboflavin is prepared matters a great deal. It was established early on (in rat corneas) that the standard Dresden protocol riboflavin preparation (0.1% riboflavin, 20% dextran T500) failed to penetrate the corneal epithelium into the stroma in any significant amounts with iontophoresis, but that the far more soluble 0.1 % riboflavin-5‘-phosphate did (18). A comparison of epi-off versus iontophoretic TE-CXL (I-CXL) was performed in rabbit eyes using a different riboflavin solution, Ricrolin+ (0.1% riboflavin, EDTA and trometadol), 1 mA for 5 minutes. That study showed that I-CXL was associated with a 45 percent lower corneal riboflavin concentration than corneas soaked using the traditional epi-off method. However, when these corneas were subjected to stress-strain assessments and challenged with collagenase digestion, both the epi-off and I-CXL-treated corneas exhibited similar median stress at 10 percent strain and similar collagenase resistance (19). Mastropasqua et al. (20) compared the concentration of riboflavin in human cadaver corneas as introduced by epi-off, TE and iontophoresis, finding that the mean riboflavin content in the superficial slice in the epi-off group was about two-fold greater than that of the iontophoresis group (50.5 ± 5.3 μg/g and 23.6 ± 2.5 μg/g, respectively) and four-fold greater than that of the TE group (11.7 ± 3.3 μg/g) (Figure 7). Clinical experience with I-CXL is beginning to be reported (Table 2), too, and it appears to tell a similar story: the cross-linking effect appears to be better than regular TE-CXL, but not as great as epi-off CXL.
One study that reported one-year results of I-CXL on 20 eyes from 20 patients with progressive keratoconus has provided some initial, encouraging results: significant improvements in corrected distance VA, with no progression noted over that period and non-significant trends toward topographic improvement (21). The study authors speculated that I-CXL “has the potential to become a valid alternative for halting the progression of keratoconus while reducing postoperative patient pain, risk of infection, and treatment time in select patients,” but noted that “the relative efficacy of this technique compared to standard epithelium-off techniques remains to be determined.”
The availability of evidence
Ultimately, it comes down to this: the evidence for epi-off CXL is a known quantity; it works and its effects persist for at least a decade (Table 3). Removing the corneal epithelium might be uncomfortable for the patient – yes, it’s a lengthier and more painful procedure than TE or I-CXL, and yes, it does carry a small increase in risk of corneal infection or other adverse events like haze. But these risks can easily be mitigated, and the pain and hazing can be managed. TE CXL – either with or without iontophoresis – would be a great option for patients with keratoconus, if it could work as effectively as epi-off CXL, but there’s just not enough proof at the moment that either epi-on technique can. Until there’s good evidence that a TE-CXL protocol can come close to the efficacy of epi-off CXL with the Dresden protocol, it’s going to remain that way.Frederik Raiskup is a senior consultant at the Carl Gustav Carus University Hospital, Dresden, Germany.
References
- LJ Davis et al., “Longitudinal changes in visual acuity in keratoconus”, Invest Ophthalmol Vis Sci, 47, 489–500 (2006). PMID: 16431941. JT Barr et al., “Estimation of the incidence and factors predictive of corneal scarring in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study”, Cornea, 25, 16–25 (2006). PMID: 16331035. RL Rebenitsch et al., “The lifetime economic burden of keratoconus: a decision analysis using a Markov model”, Am J Ophthalmol, 151, 768–773.e(2011). PMID: 21310384. A Cummings, “Constructive Cross-Links”, The Ophthalmologist, 1, 25–36 (2013). bit.ly/topcxl. Accessed February 24, 2015. A Caporossi et al., “Age-related long-term functional results after riboflavin UV A corneal cross-linking”, J Ophthalmol. 2011:608041 (2011). PMID: 21837270. A Caporossi et al., “Riboflavin-UVA-induced corneal collagen cross-linking in pediatric patients”, Cornea, 31, 227–231 (2012). PMID: 22420024. G. Wollensak et al. “Riboflavin/ultraviolet- a-induced collagen crosslinking for the treatment of keratoconus”, Am J Ophthalmol, 135, 620–627 (2013). PMID: 12719068. F Raiskup et al.,“Corneal collagen crosslinking with riboflavin and ultraviolet-A light in progressive keratoconus: ten-year results”, J Cataract Refract Surg., 41, 41–46 (2015). PMID: 25532633. JA Craig et al., “Epithelium-off photochemical corneal collagen cross-linkage using riboflavin and ultraviolet A for keratoconus and keratectasia: a systematic review and meta-analysis”, Ocul Surf, 12, 202–214 (2014). PMID: 24999102. C Koppens et al., “Refractive and topographic results of benzalkonium chloride-assisted transepithelial crosslinking”, J Cataract Refract Surg, 38, 1000–1005 (2012). PMID: 22624899. G Wollensak et al., “Biomechanical and histological changes after corneal crosslinking with and without epithelial debridement”, J Cataract Refract Surg, 35, 540–546 (2009). PMID: 19251149. G Scarcelli et al., “Brillouin microscopy of collagen crosslinking: noncontact depth-dependent analysis of corneal elastic modulus”, Invest Ophthalmol Vis Sci, 54, 1418–1425 (2013). PMID: 23361513. A Caporossi et al., “Transepithelial corneal collagen crosslinking for progressive keratoconus: 24-month clinical results“, J Cataract Refract Surg, 39, 1157–1163 (2013). PMID: 23790530. A. Kissner et al., “Pharmacological modification of the epithelial permeability by benzalkonium chloride in UVA/Riboflavin corneal collagen cross- linking”, Curr Eye Res, 35, 715–721 (2010). PMID: 20673048. A Leccisotti, T Islam, “Transepithelial corneal collagen cross-linking in keratoconus”, J Refract Surg, 26, 942–948 (2010). PMID: 20166621. G Wollensak et al., “Biomechanical efficacy of collagen crosslinking in porcine cornea using a femtosecond laser pocket”, Cornea, 33, 300–305 (2014). PMID: 24457453. AJ Kanellopoulos, “Collagen cross-linking in early keratoconus with riboflavin in a femtosecond laser- created pocket: initial clinical results”, J Refract Surg, 25, 1034–1037 (2009). PMID: 19731884. A Arboleda et al., “Evaluating in vivo delivery of riboflavin with coulomb-controlled iontophoresis for corneal collagen cross-linking: a pilot study”, 55, 2731–2738 (2014). PMID: 24667860. M Cassagne et al., “Iontophoresis transcorneal delivery technique for transepithelial corneal collagen crosslinking with riboflavin in a rabbit model”, Invest Ophthalmol Vis Sci, [Epub ahead of print] (2014). PMID: 24644053. L Mastropasqua et al., “Corneal cross- linking: intrastromal riboflavin concentration in iontophoresis-assisted imbibition versus traditional and transepithelial techniques”, Am J Ophthalmol, 157, 623–630.e1 (2014). PMID: 24321474. P Vinciguerra et al., “Transepithelial iontophoresis corneal collagen cross-linking for progressive keratoconus: initial clinical outcomes”, J Refract Surg, 30, 746–753 (2014). PMID: 25375847.
