 Figure 1. The four hatha yoga positions that were assessed for changes in IOP
Figure 1. The four hatha yoga positions that were assessed for changes in IOP
In 2001, an estimated 4 million people in the US practiced yoga; by 2011, this had become 20 million. That there are potentially serious health risks involved may therefore come as something of a surprise. Not the compression and damage to nerves and the vasculature, spinal arthritis and stenosis – injuries happen, that is the nature of exercise. The worrying, potentially pathological, change is in the eye, and it could occur any time that someone performs a headstand: a transient but dramatic doubling in intraocular pressure (IOP) (1). Of course, yoga involves much more than just headstands, so a team of researchers at the New York Ear Eye and Ear Infirmary of Mount Sinai and the Department of Ophthalmology, Columbia University Medical Center, New York, on finding themselves unable to answer the question “can I do yoga?”, decided to investigate if it was just headstands that their patients needed to avoid, or the yoga classes in their entirety (2).
“We had ten patients with glaucoma and ten controls, and we looked at four common positions that had never been tested before,” explains Jessica Jasien, lead author of the study. What they found (Figure 1) was that all four positions produce an immediate increase in IOP. “All positions increased patients’ IOP during the time that they were in the position, with the rises ranging from 20 to 74 percent,” says Jasien. The greatest increase was seen in the Adho Muka Svanasana, or downward dog position (Figure 2), one of the most commonly used positions in all of hatha yoga. The IOP elevations were “really significant for patients with glaucoma as well as controls”. There was no significant difference between the two groups in the extent of the IOP changes that resulted from each pose.
Jasien emphasises that this was a pilot study that did not look at causes. She notes however that “the head being below the heart in these positions means that venous pressure increases, and perfusion pressure decreases, which could lead to an increase in IOP.” When asked if yoga should come with a health warning for patients with glaucoma, Jasien responded emphatically. “Definitely,” she said. “We’re asking our patients to modify positions and try not to do complete inversions. We’d also encourage physicians to advise people with a history of glaucoma in their family to make their yoga practitioners aware of this.”
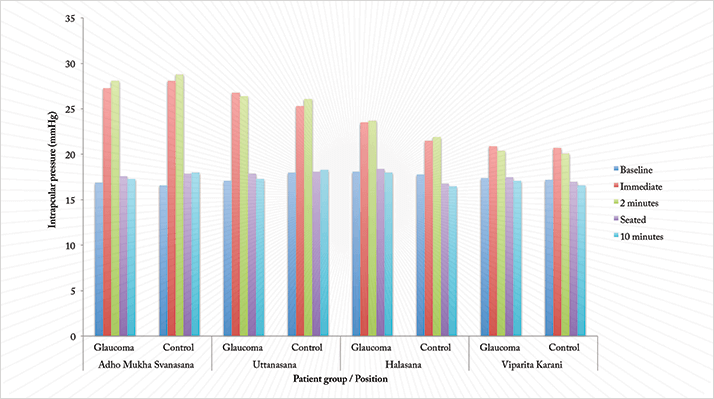 Figure 2. Patient and control IOP levels for each of the four positions, taken at baseline, immediately upon the position being achieved, two minutes into holding the position, seated immediately afterwards, and ten minutes later.
Figure 2. Patient and control IOP levels for each of the four positions, taken at baseline, immediately upon the position being achieved, two minutes into holding the position, seated immediately afterwards, and ten minutes later.
References
- M. Baskaran, K. Raman, K.K. Ramani, et al., “Intraocular pressure changes and ocular biometry during Sirsasana (headstand posture) in yoga practitioners”, Ophthalmology, 113, 1327–1332 (2006). J.V. Jasien, C.G. De Moraes, R. Ritch, “Intraocular Pressure Changes in Subjects With and Without Glaucoma During Four Common Yoga Positions”, IOVS, 55, ARVO E-Abstract 114 (2014).
