Jose Maria Martinez de la Casa, an ophthalmic surgeon based in Hospital Clínico San Carlos in Madrid, Spain, treats the full spectrum of glaucoma patients – from mild cases that can be controlled with medication to highly complex cases including advanced or refractory glaucoma. We asked him to comment on his clinical experience of the combination of cataract surgery and PRESERFLO™ MicroShunt.
What drives surgical decisions in glaucoma patients?
The determining factor is target IOP, because it encapsulates all other relevant features of the patient – including age, life expectancy, and stage of glaucoma. A range of patient-specific factors are taken into account when determining target IOP: these include baseline IOP, extent of IOP fluctuation, and the presence of conditions that may complicate surgery, such as high myopia. For example, patients whose disease is at an identical stage, but who differ significantly in age, are likely to have different target IOPs, and consequently will require different surgical approaches. Similarly, an elderly patient with advanced but very slowly progressing glaucoma will have a very different target IOP from a young patient with mild but rapidly progressing glaucoma. In short, target IOP is the key criterion when planning the clinical management of these patients.
In terms of deciding between specific techniques to achieve the target IOP, I would say that subconjunctival MIGS techniques have a very important role in the large number of patients with slowly progressing mild-to-moderate glaucoma. I also often opt for these approaches in complex patients, such as high myopes, because subconjunctival MIGS have a better safety profile than conventional surgery. Furthermore, they can be used both as a standalone technique and in combination with cataract surgery. But the final surgical choice is always made on the basis of an evaluation of multiple factors.
Describe your experience with PRESERFLO™ MicroShunt.
I began using PRESERFLO™ MicroShunt in 2013, and have now implanted it in around 70 patients. The technique is very reproducible and reliable – the only change I have made is to increase routine mitomycin C (MMC) concentration from 0.2 to 0.4 mg/ml. I’m very happy with PRESERFLO™ MicroShunt outcomes, which are very consistent. In particular, PRESERFLO™ MicroShunt has a low rate of adverse events, which makes it a good alternative to trabeculectomy in patients with mild-to-moderate glaucoma. Overall, it is simply a more stable system; postoperative results are always very similar over the first few weeks in terms of IOP reduction and follow up. In my experience, it also has lower rates of avascular blebs and needling than other subconjunctival MIGS options, and very reliable, reproducible post-operative recovery. My PRESERFLO™ MicroShunt patients also need fewer post-operative consultations than trabeculectomy – maybe two visits in the month following surgery. By contrast, trabeculectomy patients need to be seen more frequently to release sutures or perform the other interventions that trabeculectomy commonly requires. In the current pandemic, limiting patients’ repeat visits at the hospital and therefore potential infections can only be a good thing; it also gives me more time to spend with patients who need my immediate attention. Surgeons’ time is now even more precious as we attempt to make back the time lost due to the COVID-19 control measures imposed.
What are your thoughts regarding standalone or combination surgery?
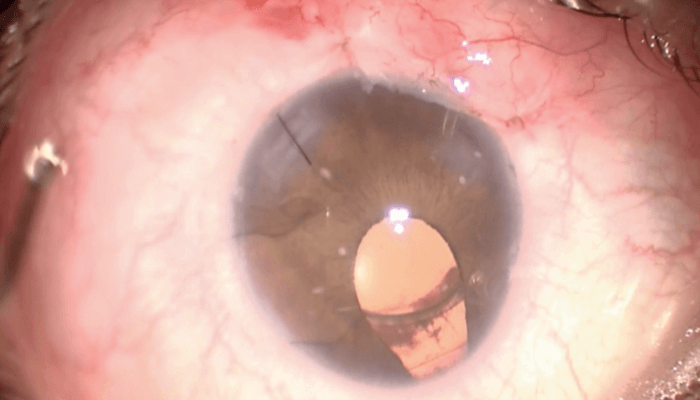
I started out employing PRESERFLO™ MicroShunt as a stand-alone procedure, but am increasingly combining it with cataract surgery; today, perhaps half of my PRESERFLO™ MicroShunt procedures are combined with cataract surgery. There are practical advantages to the combination approach; for example, in an eye with a thick lens and a narrow anterior chamber, I can remove the lens, thereby widening the anterior chamber and enabling me to implant PRESERFLO™ MicroShunt more safely – that is, further from the endothelium – than is possible when employing a stand-alone procedure on a similar eye. But even in normal cataract patients with moderate glaucoma, PRESERFLO™ MicroShunt is a very good option in terms of efficacy and post-operative follow ups.
Why PRESERFLO™ MicroShunt rather than other MIGS?
For particular patients – such as younger individuals with a thick Tenon’s capsule – PRESERFLO™ MicroShunt has advantages over other MIGS, such as XEN® (Allergan). It allows you to open up the conjunctiva and apply MMC over a wider area; to appropriately manage the Tenon’s; to implant the device such that it is covered by Tenon’s; and to better control post-operative blebs and needling frequency. And in complex patients – such as young, high myopes – it’s better than trabeculectomy, because the complication rate is lower.
Any final thoughts?
Surgeons should remember that, although PRESERFLO™ MicroShunt implantation is simple and very reproducible, it is important to maintain good technique. Key steps in a combination approach include: open the conjunctiva; apply MMC; flush out MMC; remove the cataract; insert the intraocular lens (IOL); put a stitch in the principal incision to ensure anterior chamber stability; remove viscoelastic; place PRESERFLO™ MicroShunt in the anterior chamber. Do each step correctly, including measuring the distance from the limbus, and placing the implant as far as possible from the endothelium to avoid problems such as corneal decompensation. I normally use 0.4 mg/ml MMC, but if I find that the eye has a very thin conjunctiva, without any Tenon’s, I dilute the preparation to 0.2 mg/ml. In any case, remember to flush away the MMC before cataract removal to avoid MMC going inside the eye – it is toxic to endothelium. Secondly, and very importantly, always remove all viscoelastic after IOL placement and before PRESERFLO™ MicroShunt insertion in the anterior chamber. If you bear the above in mind, and pay appropriate attention to each step in the technique, you can expect to achieve an IOP in the low teens with PRESERFLO™ MicroShunt.
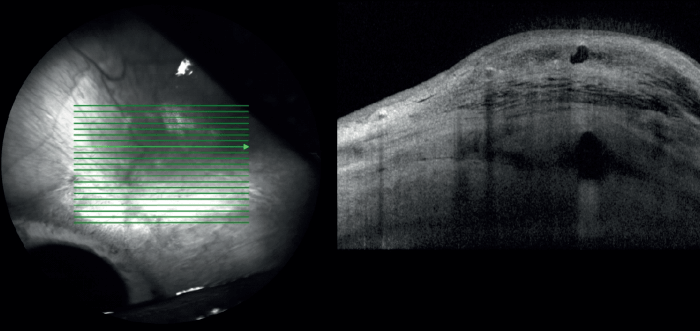
In a single patient, combined PRESERFLO™ MicroShunt and cataract surgery gives better IOP control in an eye with moderate glaucoma than is achieved with isolated cataract surgery in an eye with mild glaucoma.
• High myope, iris coloboma, thick lens, 30 mm axial length
• Right Eye: Moderate glaucoma, cataract → Combined surgery (PRESERFLO™ MicroShunt + cataract)
• Left Eye: Mild glaucoma, cataract → Cataract surgery
• Outcomes (2 years post-surgery):
• Right Eye: IOP 12 mmHg, stable glaucoma (no medications)
• Left Eye: IOP 14 mmHg (two medications)
Financial disclosures
Professor Martinez de la Casa is a speaker and consultant for Santen, Allergan, Alcon, Pfizer, Novartis, Thea, B&L, and Glaukos, a speaker for ICare and consultant for AJL and Visufarma. He has received grants from Santen, Ivantis, Allergan, Pfizer, Glaukos, and Thea.
Indication: The PRESERFLO™ MicroShunt glaucoma drainage system is intended for reduction of intraocular pressure in eyes of patients with primary openangle glaucoma where IOP remains uncontrollable while on maximum tolerated medical therapy and/or where glaucoma progression warrants surgery.
Please read the PRESERFLO™ MicroShunt Instructions for Use carefully before using the device.
The use of PRESERFLO™ MicroShunt requires a prior specific treatment by administering an antifibrotic agent according to the state of the art guidance for the surgical treatment of glaucoma. The Instructions for Use of PRESERFLO™ MicroShunt provide detailed information of the use of antifibrotic agent called Mitomycin C which was used in the studies at a dose of 0.2 mg–0.4 mg/mL and wash with a duration of 2–3 minutes. For further detailed information please consult systematically the Instructions for Use.
