Esther Hoffmann, Head of Glaucoma Department of Ophthalmology at Mainz, and Anselm Jünemann, Professor of Ophthalmology, Chairman, and Medical Director of the Department of Ophthalmology at the University of Rostock, Germany, discuss using the Kahook Dual Blade for their cataract patients.
What is your experience with using the Kahook Dual Blade (KDB)? What kind of patients do you use the tool for?
Hoffmann: I have been using the KDB for several years and I’m very happy with the tool and its capabilities. I use it for cataract patients with mild to moderate glaucoma when I need a way to lower their IOP – and, in fact, I have been able to get an additional 2–4 mmHg IOP-lowering effect for these patients. For patients before trabeculectomy, I sometimes use the KDB as a bridging therapy.
In my opinion, the KDB is one of the best tools to use for my cataract patients with glaucoma, because I have found that the canal of Schlemm tends to show blood reflux at the end of surgery. The canal of Schlemm tends to show blood reflux at the end of surgery, which signals the successful removal of the impaired outflow pathway.
Jünemann: I also find the KDB useful in combination with cataract surgery. I use it for patients with open angle glaucoma with a target pressure of around 15 mmHg. I have been able to achieve reduction to 13–15 mmHg mean IOP values while reducing patients’ medication. Gonioscopically, the angle should be graded 3–4 in the Shaffer scale.
Due to the excision of trabecular meshwork, using KDB is not just trabeculotomy, but trabeculotomy ab interno, with all the clinical advantages that entails.
What are the main advantages of the KDB in combination with cataract surgery?
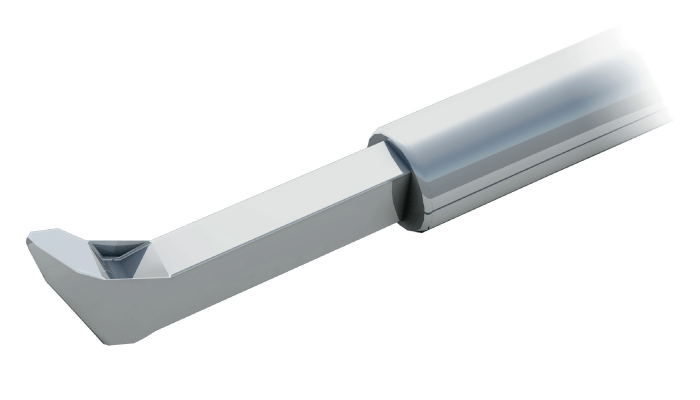
Hoffmann: First of all, the surgery is quick and easy to perform – especially if surgeons are used to performing angle surgery – with minimal trauma and, in my experience, no additional paracentesis. KDB is small and allows for “soft” removal of the trabecular meshwork by lifting and stretching the tissue and providing a smooth transition through the canal wall.
Jünemann: The KDB is a brilliant tool for mechanical trabecular excision without alteration of the surrounding tissue, especially the outer wall of the canal of Schlemm. It can be used very easily in combination with cataract surgery using existing paracentesis. I feel very confident when using the KDB thanks to its great safety profile.
Could you share any pearls for surgeons who might be thinking of starting to use the KDB?
Jünemann: To begin with, it might be helpful to select pseudophakic or phakic patients with a deep anterior chamber. Remember that trabecular pigmentation helps to identify the structures of the anterior chamber angle – take time to visualize it during surgery.
If possible, use the KDB first in combination with cataract surgery. First, because corneal alterations like edema may reduce visualization of the anterior chamber angle; second, because the excised trabecular tissue will be removed during cataract surgery. Hoffmann: You should be educated in performing gonioscopy – perform it in every patient before using KDB to visualize the canal of Schlemm and check if the angle has no goniosynechia. Also, at the beginning of your learning curve, be mindful of not pulling too much tissue.