- The posterior face of the lens capsule provides a barrier between anterior and posterior segments during cataract surgery
- Accidental rupture of the capsule causes complications but planned posterior capsulorhexis is as safe as standard surgery
- Primary posterior capsulorhexis is recommended in pediatric cataract surgery
- Some advanced lens techniques in adults also use primary posterior capsulorhexis
Do we surgeons have an irrational fear of the posterior capsule of the lens?
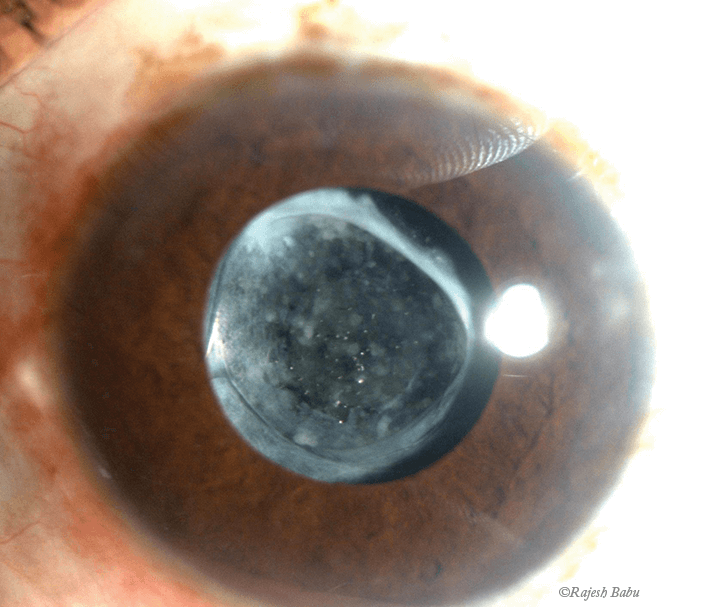
Structurally, the posterior capsule is very simple: a clear, elastic, membrane-like collagen structure synthesized by the lens epithelial cells to encapsulate the lens fibers. Functionally, however, it forms a crucial barrier between the anterior and posterior segments, both anatomically and physiologically. And it’s that barrier function that has lead us to believe that the posterior capsule should be seen and not touched. This is not without reason: accidental tearing of the posterior capsule during cataract surgery complicates lens removal, hampers the insertion of implant lenses and results in a higher rate of postoperative issues (1). In the early stages of our careers, we were constantly reminded by our seniors to guard the capsule, and most of us can remember the stress and frustration of our first few accidental posterior capsular ruptures.
My view is that, while a healthy respect for the posterior capsule is essential to ensure safe surgery, there are occasions when a controlled capsular tear can be safe – and even advantageous. One such case is in creating a primary posterior continuous curvilinear capsulorhexis (PPCCC), a useful technique that eliminates the risk of posterior capsule opacification (PCO) that sometimes occurs after “standard” cataract surgery. As post-surgical PCO complication rates are high in children (2), my preference in pediatric cataract cases is to implant a lens as primary surgery, but to perform a PPCCC before I implant the lens. In my experience, combining the PPCCC with the bag-in-the-lens (BIL) eradicates PCO. The “optic-buttonholing” technique described by Gimbel (3) and later re-introduced by Menapace works on a similar principle, albeit with some variations (4).
Encouraged by my results with children, I started to reassess how I deal with adults with straightforward cataracts. The lens that I implant has a circular optic that is inserted into the center of both the anterior and posterior capsulorhexes. Despite the fact that it is regarded by some as being a difficult and dangerous twist on a standard technique, I view the PPCCC as an essential part of the surgery. Although the additional surgical steps need to be mastered, I have found that – both in performing the technique and in teaching it – it’s no more difficult or dangerous than standard surgery, provided that the surgeon has a careful, methodical technique and understands the characteristics of the BIL implantation technique.
How to perform a PPCCC
Over the years, having performed countless PPCCCs, I have refined a technique that is simple and has served me well both in adult and pediatric cataract surgery. First, an anterior capsulorhexis is performed using a ring caliper with an internal diameter of 4.5 mm (in children) or 5.0 mm (in adults; Figure 1). The cataract lens can be removed per the surgeon’s preferred technique. Once the lens and cortex have been removed (Figure 2), I refill the anterior chamber with dispersive ophthalmic viscoelastic device (OVD). I inject over the level of the iris, as this provides a pressure balance in the anterior chamber, counteracting pressure from the posterior chamber. It also serves to flatten the capsule, giving the most predictable platform for a controlled posterior capsulorhexis. It is particularly important to fill over the level of the iris to ensure that none of the OVD enters the bag. Filling the bag would push the posterior capsule into a concave shape and makes performing the posterior rhexis more difficult and unpredictable.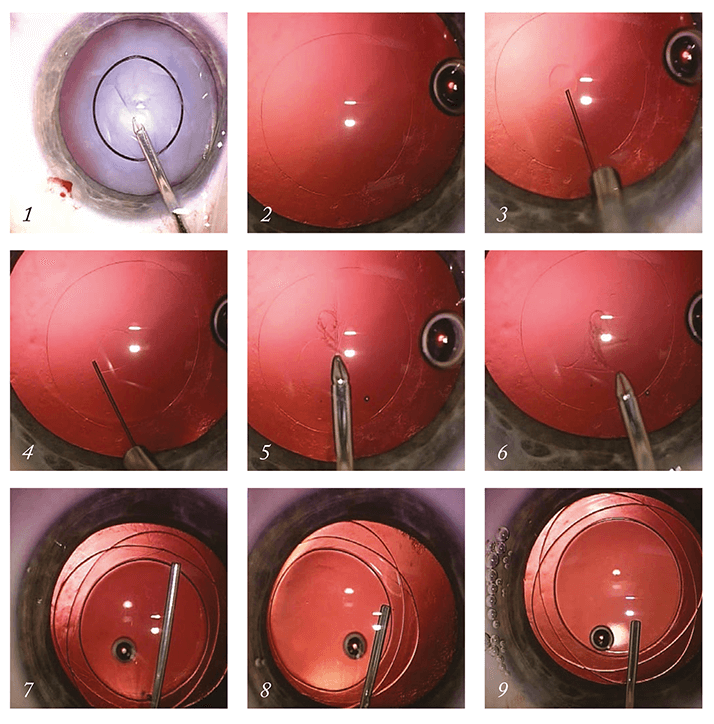
I aspirate any residual cortical fibers manually with a syringe mounted on a Helsinki cannula. The PPCCC begins with a small puncture in the posterior capsule with a 30G or tuberculin needle. At this stage, I inject Healon OVD through the small posterior capsule defect into the posterior chamber, filling the Berger's space and pushing back the anterior hyaloid face (Figure 3). The OVD gathers and forms a blister-shaped (slightly larger than the existing anterior continuous curvilinear capsulorhexis [ACCC]), providing a cushion of protection that prohibits vitreous prolapses from occurring (Figure 4). I continue the posterior rhexis with a microforceps (Ikeda Fr 2268, EyeTech), using the size of the anterior rhexis as a guide (Figures 5 and 6). For pediatric cataracts (5), the technique is modified: the initial capsular puncture is performed as described above, but the OVD injection is performed with a DORC 41 G needle (Figure 3). The bag-in-the-lens is then injected into the anterior chamber and stabilized against the anterior capsule by injection of supplementary OVD. Both anterior and posterior capsules are then glided within the lens groove at the left side (Figure 7) by exerting very delicate pressure. Then the right anterior and posterior capsules are glided within the lens groove (Figure 8), resulting in stable implantation of the BIL (Figure 9).
There are, of course, problematic cases. In patients with weak zonular fibers, the lack of counter-traction makes the posterior rhexis less predictable. Here, the insertion of a capsular tension ring after the aspiration of the last zonular fibers can provide the necessary counter-traction. I also recommend using a capsular tension ring in patients with myopia (axial lengths ≥ 26.0 mm); they typically have large capsules that require additional stabilization. I recommend this step because myopic patients are more prone to anterior vitreous schisis and have a very large Berger's space with little anterior vitreous support.
I have recently developed bean-shaped rings that can be inserted in the capsular bag or positioned in the sulcus. The inner part of the ring adapts perfectly well in the bag-in-the-lens groove, and as a result stabilizes a capsular bag/ bag-in-the-lens complex in the presence of loose zonules (6).
I have been performing a PPCCC as standard in the majority of my cataract surgeries over the last decade, and have found that (usually) no anterior vitrectomy is required. In fact, when performed correctly, there is very little disturbance of the anterior hyaloid face, and the eye retains the diffusion properties across the vitreous and aqueous interface of an eye with an intact posterior capsule – a situation most unlike that seen with accidental PC tears (7). In the long-term follow-up of these patients, my team has found that the postoperative complications were the same as that of standard cataract surgery (8). With this in mind, I advocate that all surgeons who wish expand their surgical skills and techniques learn PPCCC.
Marie-Jose Tassignon is Chief and Chair of the Department of Ophthalmology at the University Hospital Antwerp, Edegem, Belgium and University of Antwerp,
Wilrijk, Belgium.
References
- R.B. Vajpayee, et al., “Management of posterior capsule tears”, Surv Ophthalmol., 45, 473–88 (2001). A.R. Vasavada, et al., “Posterior capsule management in congenital cataract surgery”, J Cataract Refract Surg., 37, 173–93 (2011). H.V. Gimbel, T. Neuhann, “Development, advantages and methods of continuous circular capsulorhexis technique”, J Cataract Refract Surg., 16:31–7 (1990). R. Menapace, “Posterior capsulorhexis combined with optic buttonholing, an alternative to standard in-the-bag implantation of sharpedged intraocular lenses? A critical analysis of 1000 consecutive cases”, Graefes Arch Clin Exp Ophthalmol., 246, 787–801 (2008). M.J. Tassignon, et al., “Bag-in-the-lens intraocular lens implantation in the pediatric eye”, J Cataract Refract Surg., 33, 611–7 (2007). M.J. Tassignon, S.N. Dhubhghaill, “Bean-shaped ring segments for capsule stretching and centration of bag-in-the-lens cataract surgery”, J Cataract Refract Surg., 40, 8–12 (2014). V. De Groot, et al., “Lack of fluorophotometric evidence of aqueous-vitreous barrier disruption after posterior capsulorhexis”, J Cataract Refract Surg., 29, 2330–8 (2003). A. Galand, F. van Cauwenberge, J. Moosavi, “Posterior capsulorhexis in adult eyes with intact and clear capsules”, J Cataract Refract Surg., 22, 458–61 (1996).
