Diabetic retinopathy (DR) can be treated: the introduction of panretinal photocoagulation and anti-VEGF therapy over the last few years have transformed patients’ visual outcomes. But many people with DR still go on to experience vision loss and blindness, partly because of complications such as tractional retinal detachment (TRD). The treatment for TRD is pars plana vitrectomy (PPV) – perhaps one of the most complex vitreoretinal surgical procedures. Fortunate then that vitrectomy systems have undergone a great deal of development over the last decade – better fluidics, faster cut rates, modified tips and ever-smaller gauge instrumentation: 20-G gave way to 23-G; 23-G gave way to 25-G, and we now have 27-G instruments. As the gauge increases (and the instruments get smaller in diameter), in theory, so does retinal stability and the ease of manipulation of the instruments. But there’s been no direct comparisons of visual and anatomical outcomes of PPV for TRD repair using different gauge instruments – until now (1).
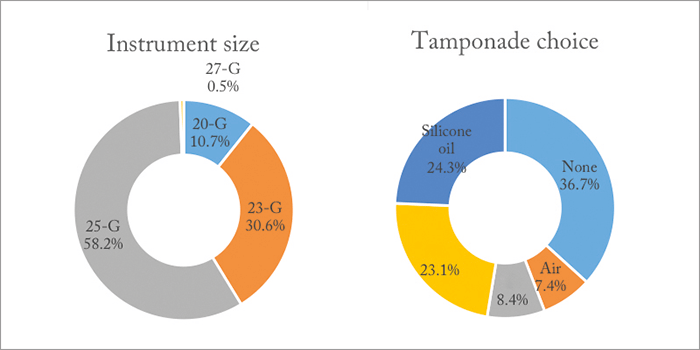
The study used an outpatient chart and operative record review from a large public eye center – the Los Angeles + University of Southern California (LA + USC) Medical Center – over a five-year period. In total, 403 eyes (from 359 patients) with diabetic TRD were included in the analysis. All patients had vitrectomy performed by either an Alcon Accurus (n=27) or an Alcon Constellation (n=376) machine, but surgical approach and choice of tamponade were based on the surgeon’s preference at the time of surgery. Baseline visual, demographic and hemoglobin A1C levels were all collected, and follow-up ranged from 0.1 to 66.9 months, averaging out at 17.5 months. The spread of instrument size and tamponade agent used during surgery is detailed in Figure 1. The outcomes? Retinal reattachment rates were good, with the vast majority of patients experiencing either improved (56.3 percent) or stable (23.8 percent) vision following surgery. Did gauge girth make a difference to the success rates? Not really. The study authors wrote: “Smaller gauge vitrectomy systems were found to have similar outcomes (p=0.73) to 20-G instrumentation” (Figure 2a).
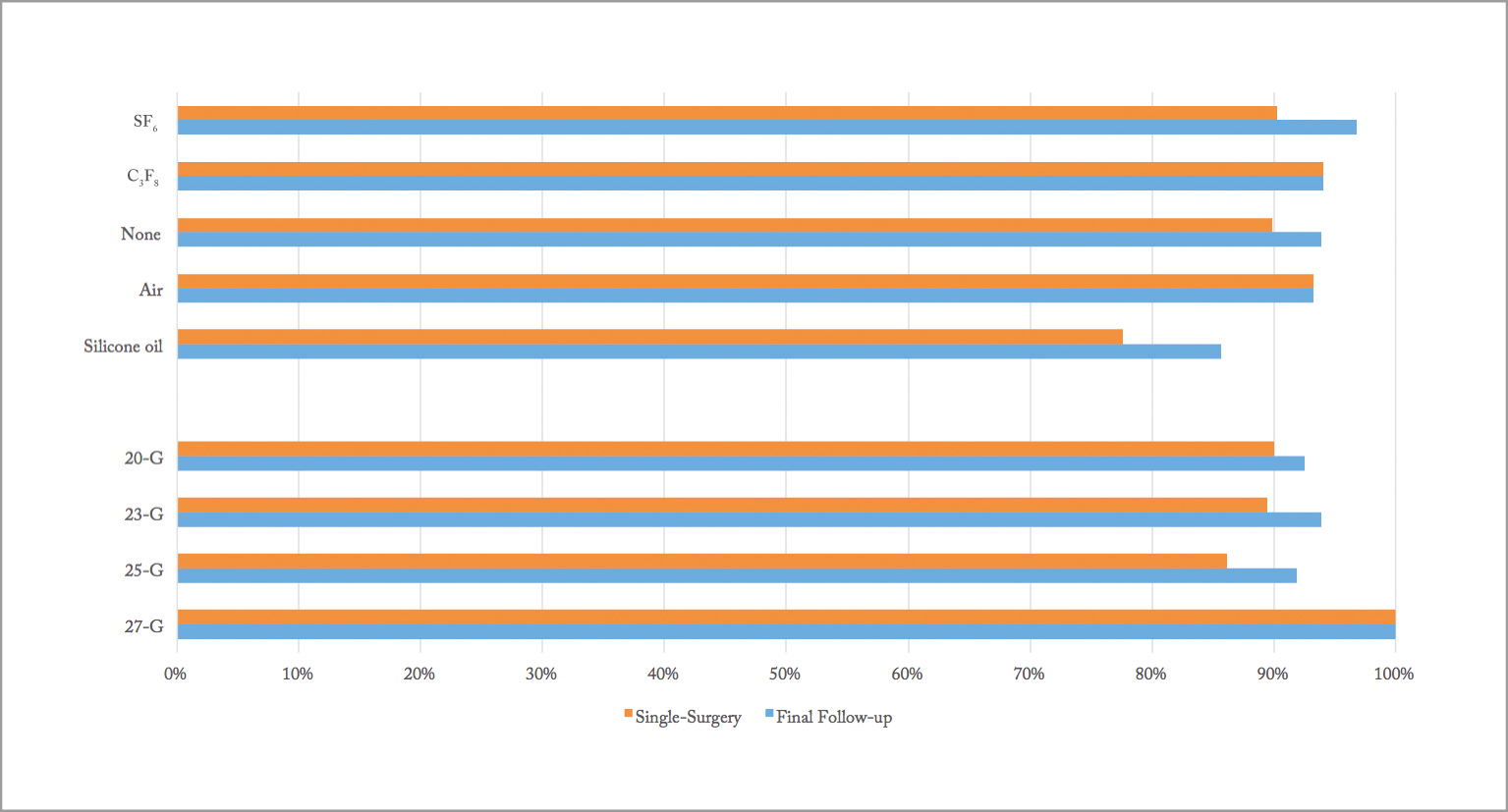
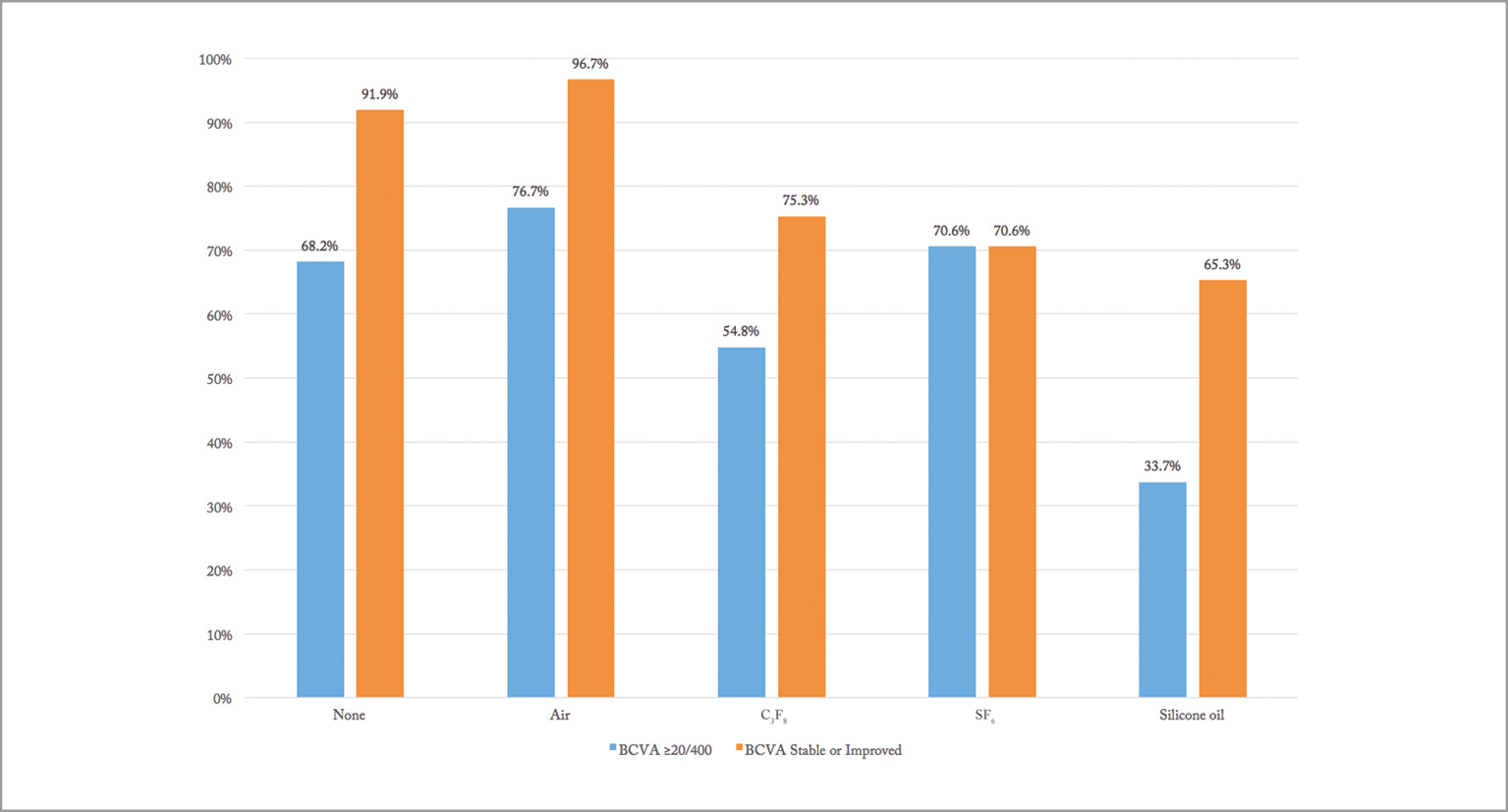
What did make a difference was the tamponade used. Patients who received silicone oil had significantly lower reattachments rates (p=0.013, Figure 2b) and significantly higher rates of vision loss (p<0.0001; Figure 3) – although these cases tended to be more challenging, as they were more likely to have concurrent rhegmatogenous and macula-involving detachments. So the answer to the age-old question of does size matter? According to this study, not as much as what you choose to do with it – “it” being the tamponade choice.
References
- PP Storey et al., “Visual and anatomical outcomes after diabetic traction and traction-rhegmatogenous retinal detachment repair”, Retina, [Epub ahead of print] (2017). PMID: 28796149.
