- We still don’t really know what glaucoma is, but dogma states that it is caused by elevated IOP
- What’s more likely is that glaucoma results from an imbalance of two pressures that act on the optic nerve: IOP and ICP – as does pseudotumor cerebri and VIIP, something that many astronauts on the international space station experience as a consequence of microgravity
- Pressurized goggles, which decouple IOP from ICP, may help to rectify this imbalance
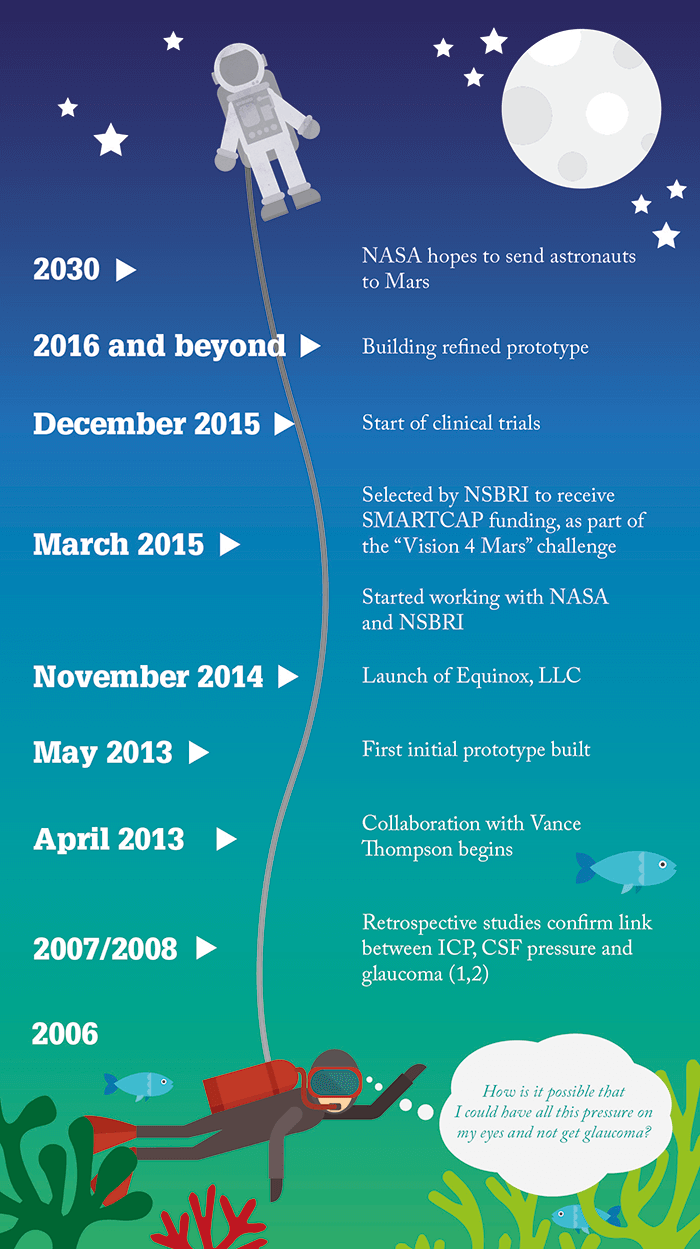
- Trials are underway to investigate the pressurized goggles for the control of eye pressure in patients with glaucoma, and future studies may help astronauts hoping to make it to Mars someday
I like to use the phrase “The dark side of the moon” when referring to glaucoma. Why? Because we have real problems with it: we don’t fully know what glaucoma is or what causes it. Just as we on Earth only see one side of the moon, we ophthalmologists have only really looked at one side of glaucoma – the eye side. The common belief is that glaucoma is a “one pressure” disease – intraocular pressure (IOP). And although IOP certainly matters in glaucoma, the reason why is not that clear.
Re-hypothesizing
My belief is that the balance between IOP and intracranial pressure (ICP), i.e. the pressure differential, is what really matters in glaucoma, not just the absolute pressure inside the eye. And reaching this hypothesis began when I was 30 feet underwater wondering why scuba divers don’t get glaucoma. At this time, I was an ophthalmology resident at Duke University Eye Center, and excited by the idea, so I presented it to one of my Professors. Their response of “You’re probably not right but you should study it,” resulted in a collaboration between Duke and the Mayo Clinic, and along with R. Rand Allingham and the late Doug Johnson, we published our first paper in 2008 (1). We performed a large retrospective analysis on over 50,000 patients who had undergone lumbar puncture over the past 20 years at the Mayo Clinic, and we compared ICP in patients who had glaucoma with those who didn’t. What we found was clear: patients with glaucoma have low ICP. Our second publication (2) showed that relative to non-glaucomatous controls, ICP was lower in patients with primary open-angle glaucoma (POAG) and patients with normal tension glaucoma (NTG), but higher in patients with ocular hypertension (OHT). So with human clinical data supporting the concept that ICP matters in glaucoma, our next step was to consider how we could use this information to actually help people. And what makes it meaningful? At this point, whilst doing my fellowship with Dick Lindstrom, I shared this information with him and he said “I think you are right. What are you going to do?” To my response of “I don’t know!” he then advised “Opportunity favors the prepared mind.” And his advice stuck with me. I kept thinking, and then one day I realized that the reason astronauts in the NASA International Space Station (ISS) were developing papilledema was probably because their ICP is higher than their eye pressure.The minus alpha
It was at this time that I and my business partner, Vance Thompson, started thinking about how to help these astronauts. Ping-ponging ideas back and forth we thought about the use of a pressurized helmet, but we realized that this would change both the eye pressure and the ICP, so the differential wouldn’t change. But what about goggles, which would relieve some pressure just on the eyes but wouldn’t affect ICP? And that’s where our idea was born. Excited by this, I set about making a prototype by ordering some goggles and a small pump, putting together tubes, and playing with them to see if I could get a seal and get the pressure to change – this was really whatever is before an alpha product! The idea was that the goggles can be used to control eye pressure, by drawing a small vacuum or applying pressure above the eye, thereby decoupling IOP from ICP. Since then, we’ve been refining the goggles; not only do they have to work but they need to be comfortable too. Our challenge at the moment is to demonstrate that we can control IOP, and we have a number of small clinical trials examining this.The clinic… and beyond
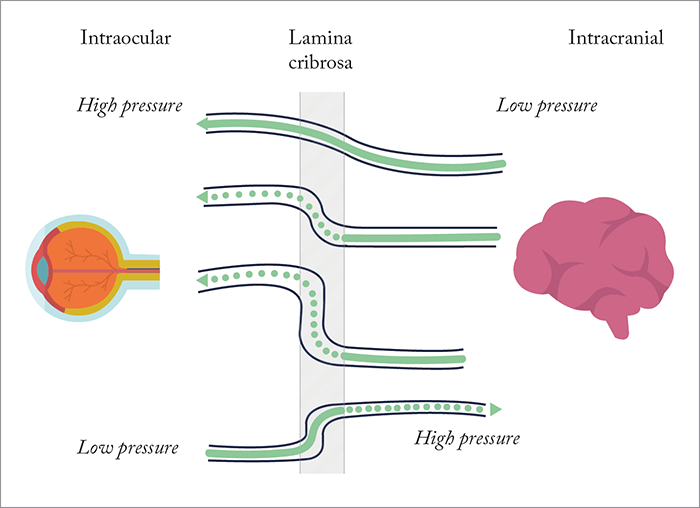
Although we are thrilled with what we see so far, we feel that there are four constituencies we need to convince. To make it to market, we need to convince regulatory bodies like the FDA and the EMA, but we aren’t yet sure what their expectations for a trial are going to be. What we really want to do is find a way to first understand if we can actually control eye pressure. And because this theory and treatment is so novel, it’s a double-edged sword: we have this really different approach to treating glaucoma, but the hard part is designing trials that are going to have to be very different from what has been done in the past. And we don’t totally know how to do this yet. We are going to need to convince doctors that this is a real treatment, and convince payers that this treatment provides a good adjunct or an alternative to current therapies. And finally, we have to convince patients that this is meaningful, and we hope to do this by letting the data lead us in the right direction. We also hope that, for the first time ever, we will be able to dial in patients’ IOPs to exactly where we need them to be. And although it would be ideal to know patients’ ICP, it isn’t totally necessary, as we could argue that it would be ideal to know patients’ ICP for any glaucoma therapy that we use right now. Currently, when we set a target IOP for a patient, we aren’t basing this on ICP, we are basing it on clinical intuition. The goggles should work the same way: we know we want to lower IOP, and we are hopeful that the goggles can do that. In 2015, we were invited to be part of the vision for Mars team on the vision impairment and ICP (VIIP) project (3). VIIP, a syndrome of globe flattening, hyperopic shift, choroidal folds, and optic disk edema, has affected almost half of the astronauts who have stayed for an extended period on the ISS. Why? In space, ICP increases at the level of the eye as there is no gravity to draw the cerebrospinal fluid (CSF) down the caudal spinal column. To put the problem in context, it’s hypothesized, given optimal orbital alignments of Earth and Mars, to take a minimum of seven months for astronauts to reach Mars. A long-term mission on the ISS is six months, and a significant proportion of ISS crew who have spent that amount of time on the space station experience (what’s thought to be VIIP-related) vision problems, such as hyperopic shifts, scotoma, cotton wool spots, choroidal folds, optic nerve sheath distension, globe flattening and optic nerve edema (3). Unless something is done, many of the astronauts heading to Mars are going to have eye disorders. To this end, we have been further developing our goggles with NASA and the National Space Biomedical Research Institute (NSBRI) to balance the microgravity-induced increases in ICP by elevating IOP, by applying a small positive pressure within the goggles, as opposed to a small negative pressure when the goggles are in use by patients with glaucoma.It’s likely that glaucoma arises from an imbalance between IOP and ICP. When IOP is increased – or ICP is decreased – a pressure differential across the optic nerve is created. We know that ICP affects the optic nerve, as we see it in pseudotumor cerebri (idiopathic intracranial hypertension); the raised ICP forces the optic nerve to bow forwards. In glaucoma, we see optic nerve cupping, likely because a high IOP and a low ICP force the optic nerve backwards. I also believe that glaucoma may be a metabolic disease. In a normal situation, axonal transport through the optic nerve delivers metabolic needs and removes metabolic waste across the lamina cribrosa. But when the IOP gets raised (or ICP is reduced), this axonal transport may get stopped at the level of the lamina cribrosa (Figure 1). In this situation, the metabolic needs of the optic nerve aren’t met, the nerve slowly withers, ganglion cell death occurs, and glaucoma ensues. The hope is that these goggles will provide adjustable control over a patient’s IOP, allowing us to balance it with ICP. For patients (on Earth) with glaucoma, we hope to remove some of the eye pressure by drawing a small vacuum (10–15 mmHg) above the eye. For astronauts, the idea is that the goggles would elevate IOP to balance the effects of elevated ICP in space.
Next steps
As well as the necessary clinical and safety trials, we also have to demonstrate that people will actually wear the goggles. We have some advantages, as the goggles are non-invasive, can be worn during sleep, and are complimentary to existing therapies. For patients taking eye drops (or who have had any type of glaucoma surgery in the past), we expect that the goggles could be a nice adjuvant to those in addition to standalone therapy – it means we have an additional tool in the toolbox to treat glaucoma. As we are probably years away from having something that is clinically available, we are excited about what the future holds. John Berdahl is an ophthalmologist at Vance Thompson Vision in Sioux Falls, specializing in cataract, corneal, glaucoma and refractive surgery. He is also Medical Director of South Dakota Lions Eye Bank, and the CEO and founder of Equinox LLC.References
- JP Berdahl et al., “Cerebrospinal fluid pressure is decreased in primary open-angle glaucoma”, Ophthalmol, 115, 763–768 (2008). PMID: 18452762. JP Berdahl et al., “Intracranial pressure in primary open angle glaucoma, normal tension glaucoma, and ocular hypertension: a case-control study”, IOVS, 49, 5412–5418 (2008). PMID: 18719086. National Aeronautics and Space Administration: Human Research Program, Human Health Countermeasures Element, “Evidence Report: Risk of spaceflight-induced intracranial hypertension and vision alterations”, July 12, 2012. Available at: http://go.nasa.gov/2baDCBA. Accessed August 11, 2016.
