Corneal collagen cross linking (CXL) with ultraviolet (UV)-A light and riboflavin is a well-established treatment for corneal ecstasias and keratoconus. But are we using it to its full potential? This was the question pondered by Geneva and Lausanne-based researchers, who believe there are other conditions that might benefit from CXL, such as pellucid marginal degeneration and peripheral ulcers. However, these diseases require decentered, eccentric illumination profiles, meaning that partially irradiating the limbus with (potentially mutagenic) UV-A light is unavoidable. Corneal limbal stem cells are needed to repair the corneal epithelium following epi-off CXL, and damage affecting their regenerative capabilities would be detrimental to recovery. So the big question was, does UV-A light harm corneal stem cells? According to the researchers, no (1).
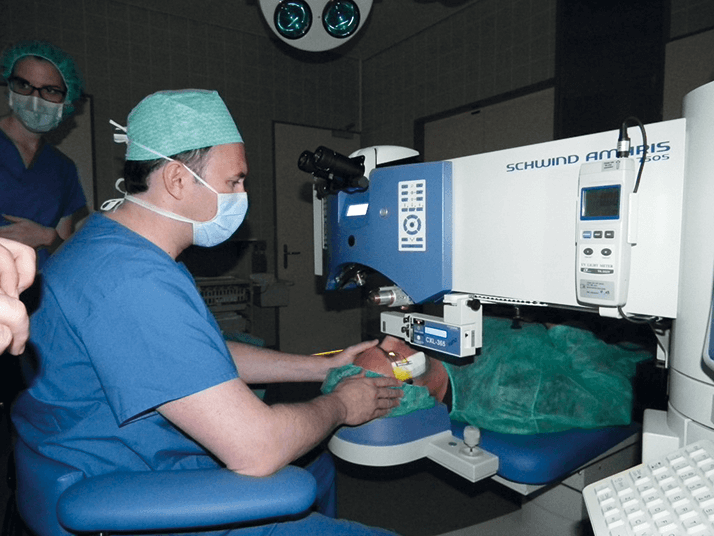
The team performed eccentric CXL using standard and double fluence (5.4 and 10.8 J/cm2, respectively) on the corneas of New Zealand White rabbits, then analyzed its effect on the corneal limbus by immunohistochemical examination of the expression pattern of the putative stem cell marker, p63. They found that UV-A radiation – at either standard or double fluence – does not affect the ability of limbal epithelial cells to regenerate, and has no effect on the expression patterns of p63, leading the study’s authors to suggest that, when eccentric CXL is “medically mandatory, a partial irradiation of the inferior limbus may be performed in the cornea without harm.” CXL has also come to the rescue of a patient with Terrien Marginal Degeneration (TMD). TMD may be rare, but it is a pernicious disease and particularly challenging to manage. By cross linking corneal collagen, CXL renders a cornea with stroma that are resistant to enzymatic degradation, which appears to hinder the corneal melting process according to a new case report (2). The patient suffered from bilateral TMD and eccentric CXL was employed in the right eye. One year later, keratometry values had decreased and both corrected distance visual acuity and corneal thickness had improved. Three years later, the patient’s left eye was treated, with similar results. Follow-up at five years showed that mean keratometric values remained stable, a reduction in maximal keratometry values, a thickening of the corneal stroma, and improvements in visual acuity were also seen. The case report authors propose that CXL shifts the balance between synthesis and catalysis of stromal collagen towards synthesis, which results in an overall increase in collagen production, augmenting the corneal stroma. The findings suggest that CXL could be used to halt – and even partially reverse – TMD-induced corneal thinning, and perhaps to prevent disease progression if used at the point of diagnosis.
References
- O. Richoz et al., “The Effect of Standard and High-Fluence Corneal Cross-Linking (CXL) on Cornea and Limbus”, Invest. Ophthalmol Vis. Sci., (2014). doi: 10.1167/iovs.14-14695. F. Hafezi et al., “Corneal Collagen Cross-linking for Terrien Marginal Degeneration” J. Refract. Surg., 30, 498–500 (2014). doi: 10.3928/1081597X-20140527-02.
