If you ask a cornea specialist, we would tell you that we want to see patients the moment they develop signs of progressive keratoconus (KC) and then intervene with corneal collagen cross-linking while the patient still has relatively normal corneas and good vision. We’d all be happy to never perform another keratoplasty (PK) procedure for KC.
But today’s reality is far from that ideal. We are still seeing KC patients identified for the first time in their 30s with high astigmatism, thin corneas – with keratometry values of 55-60 or more – and significant reductions in best-corrected vision (1). When I see a patient like this, there is always a sense of regret that they couldn’t have been diagnosed and treated earlier, before losing vision.
Put simply, stopping progression of KC in Patient A is beneficial at any stage. Frankly, that is good enough for Patient A and for me, as their doctor, to say that treatment is worthwhile. But my colleagues and I wanted to answer some harder questions: over the course of a lifetime, does the outcome of cross-linking justify its cost, when compared with conventional management with glasses and contact lenses? Is it worthwhile to society and healthcare systems? Though these may sound like cold-hearted questions, they play into the economic decisions that third-party payers and large national or private health systems have to make on a regular basis.
To find answers to these questions, we used a type of discrete-event microsimulation model that has been widely used to evaluate cost-effectiveness of medical interventions (2). It compares clinical and health outcomes and quality of life between intervention and control groups – so, in the case of our study, between eyes undergoing the FDA-approved iLink cross-linking with Photrexa Viscous (riboflavin 5’-phosphate in 20% dextran ophthalmic solution), Photrexa (riboflavin 5’-phosphate ophthalmic solution) and the KXL system (Glaukos) versus not undergoing cross-linking treatment. Patient-level microsimulation is complex, but it allowed us to model the impact of individual patient and eye histories on keratoconus progression and adjust future risks (such as the probability of PK or of graft failure) accordingly.
We simulated outcomes for both eyes of 2,000 individual patients over a lifetime horizon, using data from the US multicenter phase III pivotal trials that led to FDA approval of iLink to define the characteristics of the preoperative population (3). Data from that study and elsewhere in the published literature on the natural history of keratoconus was used to account for a variety of factors affecting disease progression, such as the impact of age on the rate of progression. Rates of anticipated adverse events associated with penetrating keratoplasty (graft rejection/failure, cataract, glaucoma) were also derived from the literature.
All of this led to a baseline age of 31 years for the modeling and a mixed population with a ratio of slow to fast progressors of 4:1.
- 26 percent reduction in the rate of penetrating keratoplasty
- 28 fewer years spent in the advanced stages of keratoconus
- Gain of 1.88 quality adjusted life years (QALYs)
- Average patient savings of $8,677 in direct costs
- Average patient lifetime savings of $44,000
- National savings of between $150 million and $736 million
- Cost savings for insurers within 4.5 years
Simulation results
We found that treatment with cross-linking results in a 26 percent reduction in the rate of PK and 28 fewer years spent in the advanced stages (Amsler-Krumeich stage 3-4) of the disease (4).
Imagine the consequences for daily function, independence and productivity of avoiding nearly three decades of meaningful visual disability! We found that treatment conveyed, on average, 1.88 more quality-adjusted life years (QALYs). QALY, a cost-utility measure commonly used in health economics studies, is a combined measure of how long the treatment will extend life and the expected quality of life during those years. Estimates of the value of 1 QALY in the US vary from $50,000 to $150,000. When the cost of the intervention is well below the value gain (and cross-linking costs far less than 1.88 x $50,000, let alone $150,000) we can consider it to be highly cost effective.
According to our modeling research, cross-linking saves everyone money! Patients experience lower direct medical costs, with average savings of $8,677. Including the cost of lost productivity, which is known to be affected in KC (5), the lifetime saving is nearly $44,000. Nationally, this translates into a savings of between $150 million and $736 million, depending on one’s estimate of prevalence. From the payer perspective, cost savings are achieved within 4.5 years.
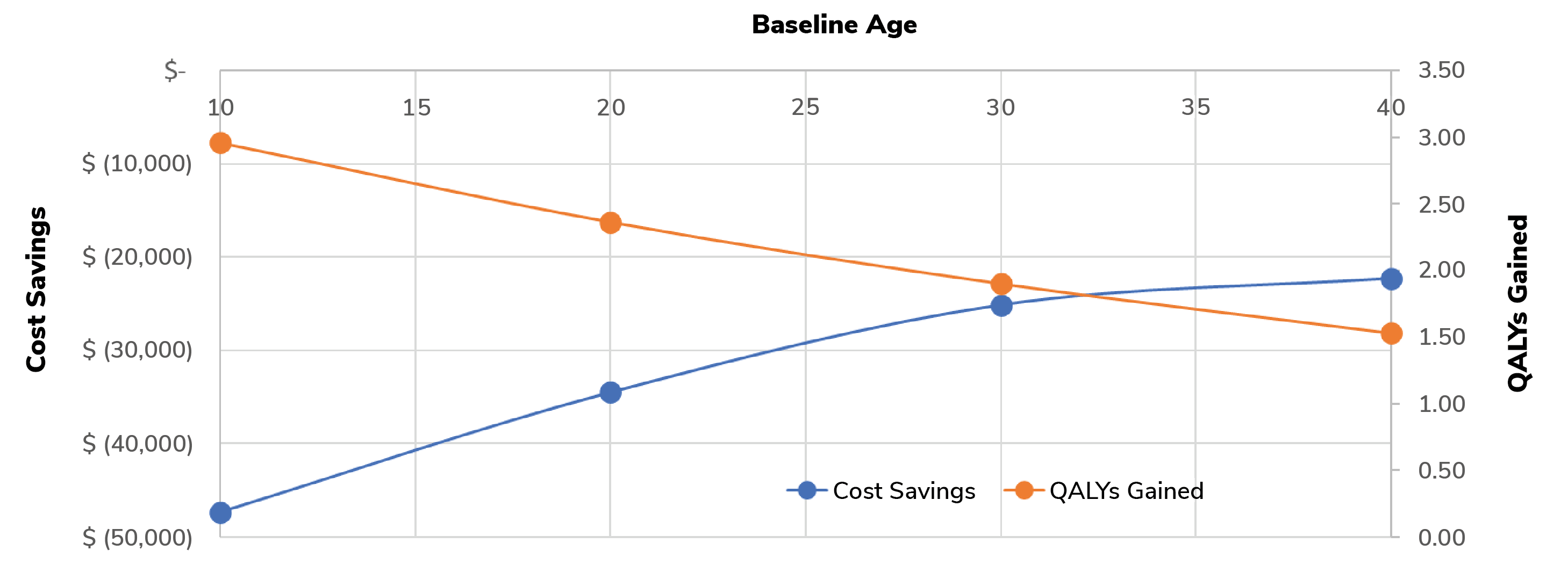
Scenario analyses in the modeling, in which the baseline age was varied, demonstrated that iLink intervention at a younger age maximized both cost savings and QALYs gained for each individual patient (see Figure 1). In fact, earlier intervention is so impactful that not only do patient productivity and quality of life improve, but the associated economic burden of progressive keratoconus on the country’s healthcare system can also be significantly reduced.
Our study has some limitations. Primarily, we relied on existing literature data to build our microsimulation model; because we based the clinical effectiveness of the iLink procedure on the 12-month results of the phase III clinical trials, the long-term benefits were also extrapolated from this short-term outcome.
However, the cold, hard numbers show that cross-linking is a win, not just for patients and their advocates, but also for third-party payers and society at large. And that’s not surprising – treatment of other progressive conditions, such as glaucoma, hypertension, and diabetes, is also cost-effective when we weigh the modest costs of treatment against higher-cost late-stage surgical interventions and many years of potential disability. Unfortunately, when it comes to keratoconus, the message isn’t getting through as loudly as my co-authors and I would like.
I am optimistic that we will see earlier diagnosis and referrals for treatment in the future, driven in part by changing approaches to the epidemic of childhood myopia. With new options to slow the progression of myopia, I think primary eye care providers will soon be capturing many more younger myopes at age five or six and treating them with behavior modification, specialized glasses and contact lenses, and topical pharmaceuticals, such as low-dose atropine. Out of all those mildly progressing myopic children, some will begin to develop asymmetrical and non orthogonal astigmatism as they reach their teen years. But because they are being regularly followed for myopia, we’ll be able to diagnose KC and cross-link them earlier, preventing advanced KC. I look forward to that day.
Educate referral network about red flags for KC, such as unexplained failure to correct to 20/20 and rapidly changing astigmatism.
- Provide rapid access to tomography/topography when KC is suspected
- Educate referring doctors about the benefits of cross-linking for patients with progressive keratoconus
- Be sure to send cross-linked patients back to their referring doctor for ongoing care and monitoring
- Refer specialty contact lens fits to local optometrists
- Remind patients and referring doctors that immediate family members of KC patients should also be screened.
- Develop relationships with doctors providing myopia control care, as they will be seeing the at-risk population (young progressing myopes) consistently from an early age.
References
- EO Kreps et al., “Diagnostic patterns in keratoconus,” Cont Lens Anterior Eye, 44, 101333 (2020). PMID: 32448765.
- JJ Caro, J Möller, “Advantages and disadvantages of discrete-event simulation for health economic analyses,” Expert Rev Pharmacoecon Outcomes Res, 16, 327 (2016). PMID: 26967022.
- PS Hersh et al., “United States multicenter clinical trial of corneal collagen crosslinking for keratoconus treatment. Ophthalmology,” 124, 1259 (2017). PMID: 28495149.
- RL Lindstrom et al., “Corneal cross-linking versus conventional management for keratoconus: a lifetime economic model,” J Med Econ, 124, 1259 (2017). PMID: 28495149.
- E Chan et al., “Economic impact of keratoconus using a health expenditure questionnaire: A patient perspective,” Clin Exp Ophthalmol, Clin Exp Ophthalmol, 48, 287 (2020). PMID: 31867844.
