One fascinating aspect of ophthalmology is its rapid pace of transformation. In the past decade, we have witnessed remarkable advancements in treating diseases that once had limited therapeutic options. Keratoconus (KC) is no exception, and I would like to share some of the newest developments in the field. Perhaps the biggest change is that we have moved beyond solely trying to address disease progression. For over two decades, ophthalmologists have had the rightly famous “Dresden protocol” method (1) for performing corneal cross-linking (CXL). Epithelium removal, saturation of the stroma with 0.1% riboflavin, followed by 30 minutes of 3 mW/cm² ultraviolet-A (UV-A) irradiation strengthens the cornea and slows, or, more often, halts the progression of the ectasia. But this is slow. In theory, increasing the UV intensity with modern LED UV light sources should decrease the time needed to deliver the total UV energy (fluence), and accelerate the cross-linking process. But for many years, in practice, we couldn’t accelerate CXL without losing a certain degree of strengthening efficacy (2).
We discovered almost a decade ago that if you try to accelerate the delivery of the Dresden protocol fluence (5.4 J/cm²), you rapidly run out of oxygen, which turns out to be an essential component of the UV-riboflavin photochemical reaction (3). However, there is good news: our research group developed a new epithelium (epi)-off protocol that is fast and just as strong as Dresden. We now have a 10 J/cm² protocol that requires 9 minutes 15 seconds of UV irradiation; three times faster than Dresden and equally strong (4). This is the protocol I use most in children, in adolescents, or in cases where I need a strong cross-linking effect. This is undeniably good news – we have already published the early rounds of laboratory data and we’re preparing to publish 2-year follow-up clinical data to further validate our initial findings.
Another area that has shown promising progress is the treatment of ultra-thin corneas. As you’re well aware, to protect the corneal endothelium Dresden protocol CXL isn’t performed on corneas thinner than 400 µm. So what do you do with an extremely thin, ectatic cornea?
Let’s revisit the two protocols we’ve relied on in the past. Our group in Zurich introduced the use of hypo-osmolar riboflavin to cause corneal swelling (5), and a few years later, Soosan Jacob proposed the use of a riboflavin-soaked specialized contact lens for these thin corneas (6). Neither artificial thickening technique is ideal. Swelling the cornea might give good results from a biomechanical point of view, but some corneas swell lots and others don’t at all. In other words, you always risk facing a surprise in the OR. If there’s one thing ophthalmologists don’t enjoy, it’s that. Contact-lens assisted CXL resulted in a ~30% loss of the cross-linking strengthening effect. But something about artificially thickening the cornea doesn’t make sense. I feel like I’m telling the patient, “My technique can only do this, so please adapt you and your condition to my technique.” Why can’t I do the opposite and adapt the technique to the cornea? I think you’ll agree this makes much more sense…
Asking this question played a pivotal role in the development of the sub400 individualized cross-linking approach. The algorithm underpinning this approach was published six years ago (7), and serves as the foundation for our protocol. It’s used to calculate the reduction in fluence required to safely cross-link thinner corneas. The clinical validation of this approach is published in the American Journal of Ophthalmology, and provides ophthalmologists with a simple, standardized and reliable framework to cross-link thin corneas (8).
A critical step in this process occurs after the corneal abrasion and riboflavin introduction – the measurement of corneal thickness using an ultrasound pachymeter. By analyzing the resulting topographic map, the location of the thinnest point becomes evident. Suppose, for instance, the thinnest point measures 280 µm. All clinicians need to do is look up our publication, which we have made accessible to everyone via the Light for Sight Foundation’s website, and see how many minutes of UV irradiation are required for the measured corneal thickness. Using the 280 µm thickness example, the ophthalmologist needs to deliver 5 minutes of UV irradiation at 3 mW/cm². It works like a charm and is an integrated cross-linking protocol in the C-eye cross-linking device.
Next, let's delve into epi-on cross-linking. The Dresden protocol requires epithelial debridement, as simple riboflavin solutions would not otherwise pass and enter the stroma. However, this brings significant downsides, including patient discomfort and an elevated risk of infection. This requires patients be diligently managed after the procedure until the epithelial cells have regrown and the roughly 8-mm hole made at the start of the procedure is closed.
How can we achieve both an intact epithelium and a robust cross-linking effect? Can we eliminate the need for corneal abrasion? Others have used penetration enhancers (to weaken the epithelium intra-cell tight junctions) or iontophoresis (to electrostatically force riboflavin across the epithelial cells) to get the riboflavin to the cornea, and supplemental oxygen to compensate for the oxygen absorbed by the epithelium that remains present. We finally found a way without depending upon either oxygen goggles or iontophoresis to make epi-on work.
How? Throughout the entire COVID-19 pandemic, we were working away at the multiphoton microscope at the Swiss Federal Institute of Technology (Figure 1). We found a way to not only get rid of the supplemental oxygen requirement, but also the need for iontophoresis. So now we have no abrasion, no increased risk of infection, and no need for extra oxygen or iontophoresis. This breakthrough, after ten years of research, was like putting the pieces of a puzzle together. We are now at the point where we can use atmospheric air – no supplementary oxygen required. We use what we call “second-generation” penetration enhancers, which allow the riboflavin to penetrate the epithelium, and a special pulsed, slow irradiation, high-fluence cross-linking protocol. According to our published laboratory data, we are as efficient in strengthening the cornea as the 10 minute / 9 mW/cm² accelerated epi-off CXL protocol.
The last topic to mention here is the evolution of second-generation customized keratoconus treatment. As I’m sure readers will know, seven years ago, the initial research on customized cross-linking was published by the group of Theo Seiler Sr. (9). The data was extremely interesting, with progressive flattening of up to nearly 3 D occurring over the months after the procedure. This was achieved by delivering UV irradiation with a device that incorporated an eye tracker and delivered different irradiation intensities to different zones of the cornea. This resulted in increased irradiation over the cone, and progressively less irradiation moving outward.
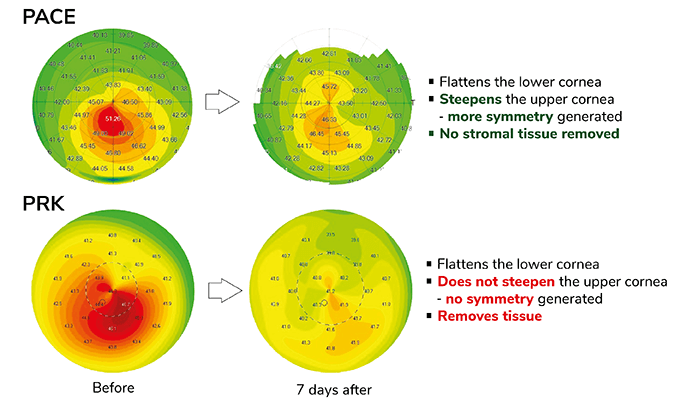
Unfortunately, the technique requires a bulky, pricey and stationary device, and so our team wondered: can we do better? Enter PACE: phototherapeutic keratectomy (PTK)-Assisted Customized Epi-on cross-linking. We have achieved almost twice the flattening effect as first-generation customized CXL, and we do this by combining CXL with an epithelial map-guided PTK. And as you can see in the images in Figure 2, the results are extremely promising. The refraction is essentially stable, we have a flattening of almost 5 D, a coupling effect, steepening of 2 D. So 5 + 2 is a regularization of 7 D in just 2 weeks, and accordingly, visual acuity increases; note how symmetric the cornea topography is over the pupil area (Figure 2).
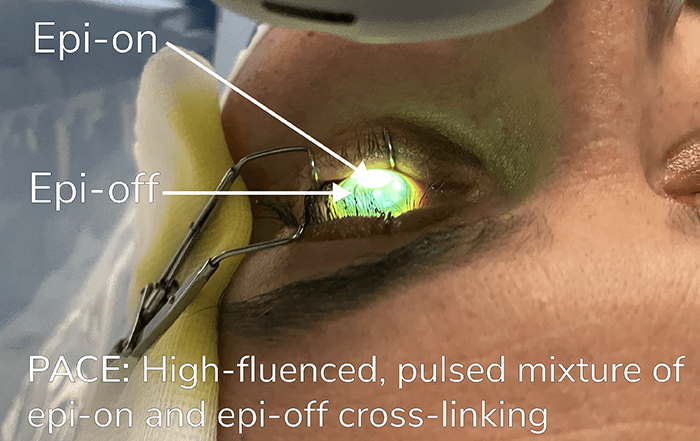
How did we do this? We did not use an eye tracker. We used a mixture of epi-off and epi-on cross-linking (Figure 3). We performed a small epithelial map driven PTK just over the tip of the cone, and then we put riboflavin onto the cornea to enhance penetration through the epi-off area. This created both epi-off and epi-on areas, and this results in a riboflavin gradient between these areas. This gradient is very useful, because we can treat a single cornea and achieve different cross-linking efficacies in different areas, thanks to the riboflavin gradient and epithelium status.
By flattening the cone so much, you drive patients towards hypermetropia, so we find that patients who are myopic – roughly in the range of 53–55 D – are excellent candidates for PACE technology. We are still finalizing and refining the technique, but I am happy to confirm that we see a rapid, mean flattening of approximately 5 D, without issue. With these results and this cornea strengthening technique, then this raises the possibility of performing a wavefront-guided photorefractive keratectomy (PRK) 6–12 months later, if needed. Currently, we are focused on determining the stabilization timeframe. How rapidly do the results manifest? When does stabilization commence? Once the corneal topography is stable, wavefront-guided PRK interventions become possible.
As we continue to refine and perfect these new techniques (along with the technology to implement them correctly) we can expect one more change: even better outcomes for our patients.
References
- Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135(5):620-627. PMID: 12719068
- Hammer A, Richoz O, Arba Mosquera S, Tabibian D, Hoogewoud F, Hafezi F. Corneal biomechanical properties at different corneal cross-linking (Cxl) irradiances. Invest Ophthalmol Vis Sci. 2014;55(5):2881-2884. PMID: 24677109
- Torres-Netto EA, Kling S, Hafezi N, Vinciguerra P, Randleman JB, Hafezi F. Oxygen diffusion may limit the biomechanical effectiveness of iontophoresis-assisted transepithelial corneal cross-linking. J Refract Surg. 2018;34(11):768-774. PMID: 30428097.
- Abrishamchi R, Abdshahzadeh H, Hillen M, et al. High-fluence accelerated epithelium-off corneal cross-linking protocol provides Dresden protocol-like corneal strengthening. Transl Vis Sci Technol. 2021;10(5):10. PMID: 34542574.
- Hafezi F, Mrochen M, Iseli HP, Seiler T. Collagen crosslinking with ultraviolet-A and hypoosmolar riboflavin solution in thin corneas. J Cataract Refract Surg. 2009;35(4):621-624. PMID: 19304080.
- Jacob S, Kumar DA, Agarwal A, Basu S, Sinha P, Agarwal A. Contact lens-assisted collagen cross-linking (Cacxl): A new technique for cross-linking thin corneas. J Refract Surg. 2014;30(6):366-372. PMID: 24972403.
- Kling S, Hafezi F. An algorithm to predict the biomechanical stiffening effect in corneal cross-linking. J Refract Surg. 2017;33(2):128-136. PMID: 28192592
- Hafezi F, Kling S, Gilardoni F, et al. Individualized corneal cross-linking with riboflavin and UV-A in ultrathin corneas: the sub400 protocol. Am J Ophthalmol. 2021;224:133-142. PMID: 33340508
- Seiler TG, Fischinger I, Koller T, Zapp D, Frueh BE, Seiler T. Customized corneal cross-linking: one-year results. Am J Ophthalmol. 2016;166:14-21. PMID: 26944278.
