- All LASIK surgeons encounter occasional complications during surgery
- LASIK is an excellent procedure and patients can still achieve great outcomes after complications
- I deal with intraoperative complications using a ‘what went right?’ method
- I overview my method and detail scenarios of different LASIK flap complications.
There is just no way around the fact that as a surgeon, you will run into complications. Managing these complications can lead to stressed surgeons, which can ultimately lead to poor outcomes and unhappy patients. Intraoperative complications can be the most challenging, as situations have to be assessed and decisions made very quickly – and seconds can really make a difference during LASIK procedures. It’s why recognizing the potential issues and managing them successfully is so important. I’d like to share my ‘what went right?’ method, and discuss how it has helped me approach and manage intraoperative LASIK flap complications – and how it might help you too.
When problems strike
Flap complications can vary depending on whether you use a microkeratome or a femtosecond laser (see Intraoperative flap complications). They can be as seemingly benign as epithelial defects or an opaque bubble layer, or more serious and ‘gut-sinking’ like buttonholes or vertical gas breakthrough. Whatever happens, surgeons need to keep calm and carry on, to try to achieve the best possible outcome. One thing that keeps me calm every time I walk into the laser vision correction suite is that literature is on our side. Many studies and reviews indicate that complication rates are low, and you can still have excellent outcomes if these are managed correctly (1)(2)(3)(4)(5). In the suite, my ‘what went right?’ method helps me stay calm and logically approach issues that may arise. The method is kind of a take on the ‘compliment sandwich’. At the moment of complication, take a step back to consider and remind yourself what has gone right and what might be in your favor. Then critically assess what has gone wrong, before looking to what is going right and how you can fix the problem to achieve the best outcomes for your patient. Of course, it’s not always as simple as that because we all manage complications differently – that’s the art of surgery. Here, I demonstrate specific examples of an incomplete flap and suction loss, and discuss how my ‘what went right?’ method helped me during – and after – surgery.Scenario 1 – Incomplete flap
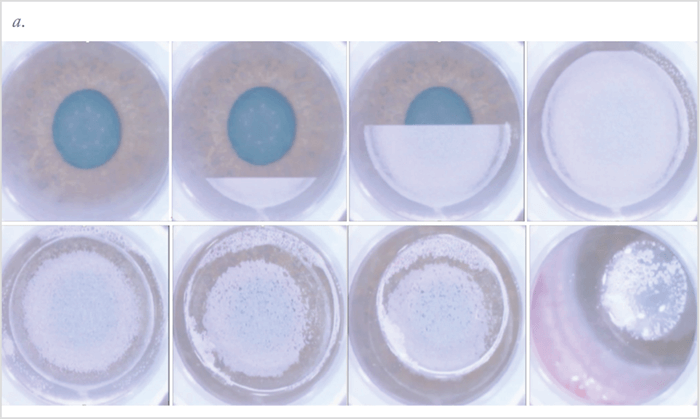
- Performing LASIK on a patient, I suddenly got a pit in my stomach towards the end of making the flap (Figure 1a).
- Instead of immediately thinking the worst, I tried to think about what went right: the meniscus remained constant, and I could see a large round raster pattern that appeared quite circular.
- Next, I considered what went wrong? Bubbles to the infero-temporal aspect and a side cut beyond my raster pattern.
- How did I keep calm and carry on? I considered what went right, and what was in my favor: this patient was having a low myopic treatment with a small optical zone – as I tend to create larger flaps (around 9 mm) the optical zone should not be close to this irregular edge.
- Completing the case (Figure 1b); I started dissecting the flap on the side where I knew my raster pattern and side cut were normal. Coming from all angles, I was able to dissect carefully under most of the flap without issues. There was some incomplete dissection (about one clock hour) but I was able to complete the side cut with Vannas scissors. The stromal bed looked great and I was able to proceed with the case – and the patient had a great outcome.
- If I hadn’t been successful at achieving the flap lift, I’d have placed it back down, waited two weeks to confirm refractive and topographic stability then performed an advanced surface ablation.
Scenario 2 – Suction loss
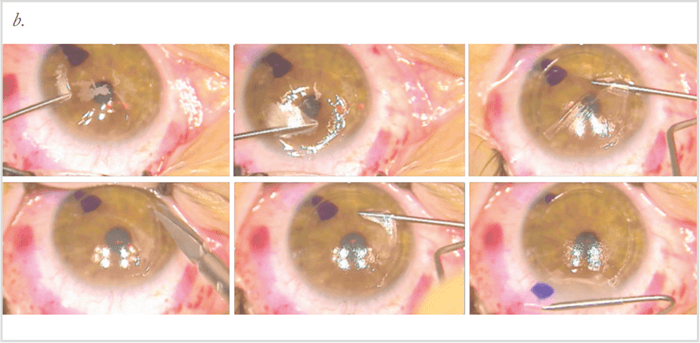
Suction loss is an uncommon (but not rare) complication that tends to occur more frequently in less-experienced surgeons. Known risk factors include small palprebral fissures, flat corneas, deep set eyes, patient/eye movement, large pterygia and redundant conjunctiva. Suction loss can provoke much anxiety – and it can happen very quickly. With the microkeratome flap, it is more likely that the procedure will be abandoned. But when using a femtosecond laser, it is possible to repeat suction and re-attempt the raster.- My patient had quite deep sockets – and was also very anxious. During the raster pattern, I kept experiencing suction loss; we achieved a complete flap after the fourth suction attempt and second femtosecond pass (Figure 2).
- What went right? I was able to achieve suction and complete the flap.
- What went wrong? It was very traumatic for my patient. At the six and 12 month visits, he was still telling me he found the experience challenging.
- What could have gone better? Looking back and considering how anxious my patient was, it might have been better to abandon the procedure, and convert to advanced surface ablation. However, he was not consented to change to advanced surface ablation, and as he had received Valium it would not have been appropriate to consent the change at the time. His preference at the time was to continue with the attempts.
- Based on this experience, I now consent my high risk patients for possible advanced surface ablation at the time of LASIK. Therefore, the patients know it may be a possibility, and if we reach the point where things become too difficult, we can convert to the procedure.
Intraoperative flap complications
Microkeratome- Epithelial defects
- Incomplete flap
- Decentered flap
- Thick/thin flap
- Suction loss
- Free cap
- Buttonhole
- Epithelial defects
- Opaque bubble layer
- Decentered flap
- Thick/thin flap
- Suction loss
- Flap tears
- Anterior chamber gas bubble
- Vertical gas breakthrough
Conclusion
We know that LASIK is a safe procedure with good outcomes – even in the face of complications. In my experience, when issues arise it really is helpful to consider what has gone right before working out how to fix what has gone wrong. It is also useful to assess how to make things go ‘more’ right. In my case, I ended up making a positive change to my LASIK practice, which will benefit future patients. If my ‘what went right?’ method resonates with you, please adopt it! Otherwise, keep calm and carry on! Priyanka Sood is a Chief of Ophthalmology at Emory Midtown Hospital, and a cornea, cataract and refractive specialist at Emory Eye Center, Atlanta, GA, USA.References
- M Ito et al., “Risk factors and retreatment results of intraoperative flap complications in LASIK”, J Cataract Refract Surg, 30, 1240–1247 (2004). PMID: 15177598. T Kohnen et al., “Short-term complications of femtosecond laser-assisted laser in situ keratomileusis cuts: Review of 1210 consecutive cases”, J Cataract Refract Surg, 42, 1797–1803 (2016). PMID: 28007112. AM dos Santos et al., “Femtosecond laser-assisted LASIK flap complications”, J Refract Surg, 32, 52–59 (2016). PMID: 26812715. M Tomita et al., “Management and outcomes of suction loss during LASIK flap creation with a femtosecond laser”, J Refract Surg, 28, 32–36 (2012). PMID: 22149663. DN Shah and S Meiki. “Complications of femtosecond-assisted laser in-situ keratomileusis flaps”, Semin Ophthalmol, 29, 363–375 (2014). PMID: 25325862.
